When a worker gets hurt on the job, the goal is simple: get them back on their feet as quickly and safely as possible. But behind the scenes, there’s a quiet revolution happening in how those injuries are treated-with generic substitution playing a central role. In 2025, more than 90% of prescriptions in workers’ compensation cases are for generic drugs. That’s not just a trend-it’s now the standard. And if you’re an employer, a claims adjuster, a nurse, or even an injured worker, you need to understand why this matters.
Why Generic Drugs Are the New Normal in Workers’ Comp
Generic drugs aren’t cheap knockoffs. They’re FDA-approved copies of brand-name medications, with the same active ingredients, strength, dosage, and how they work in your body. The law requires them to be bioequivalent-meaning they deliver the same clinical effect. Yet, they cost about 80% less. A $100 brand-name painkiller? The generic version? Around $20. That’s not a guess-it’s what myMatrixx data showed between 2014 and 2019. Meanwhile, brand-name drug prices jumped 65% in the same period, while generic prices dropped 35%. In workers’ compensation, where pharmacy costs make up about 20% of total medical spending, those savings add up fast. Multiply that across thousands of claims each year, and you’re talking millions in avoided costs. States like California and Colorado have pushed this even further. California hit 92.7% generic use by 2022. Colorado now requires 95% generic substitution for drugs on its official formulary, starting in January 2024.How It Works: The Rules of Substitution
It’s not as simple as swapping a pill at the pharmacy. Each state has its own rules. Thirty-eight states have formal drug formularies-official lists of approved medications. In states like Tennessee, the law is clear: an injured worker gets a generic drug unless the doctor writes a specific medical reason for the brand name. That reason can’t be “the patient prefers it.” It has to be clinical-like a documented allergy, a failed trial of the generic, or a narrow therapeutic index drug where small changes in dosage could cause harm. Pharmacy Benefit Managers (PBMs)-companies like OptumRx, Express Scripts, and Prime Therapeutics-handle the actual substitution. They run formularies, require prior authorizations, and flag prescriptions that don’t follow the rules. These three PBMs control about 65% of the workers’ comp pharmacy market. They don’t just push generics because they’re cheaper-they’re required to by state law and contract. The Orange Book, published by the FDA, is the bible here. It lists every approved generic and rates its therapeutic equivalence to the brand. If a generic is rated “AB,” it’s fully substitutable. If it’s “BX,” substitution isn’t recommended. Doctors and pharmacists use this daily.What’s Holding Back Full Adoption?
Despite the numbers, resistance still exists. A 2021 survey by the American College of Occupational and Environmental Medicine found that 73% of occupational health providers say patient skepticism is their biggest hurdle. Many injured workers believe brand-name drugs are stronger, safer, or more effective. They’re not. But that belief is deep-rooted. One nurse told me she once had a worker refuse a generic pain patch because he thought it was “fake medicine.” After showing him the FDA label and explaining bioequivalence, he agreed to try it-and reported the same relief. There are also real, though rare, exceptions. For drugs with a narrow therapeutic index-like warfarin or certain seizure medications-even tiny differences in absorption can matter. That’s why substitution isn’t automatic for these. But these cases make up less than 2% of all workers’ comp prescriptions, according to Coventry’s data. Another issue? The generic market itself isn’t always competitive. Enlyte’s 2022 analysis found that some generic manufacturers have colluded to limit supply or raise prices-especially for older drugs with few competitors. That’s led to shortages and unexpected spikes in cost, even for generics. It’s ironic: the system designed to cut costs can sometimes be gamed.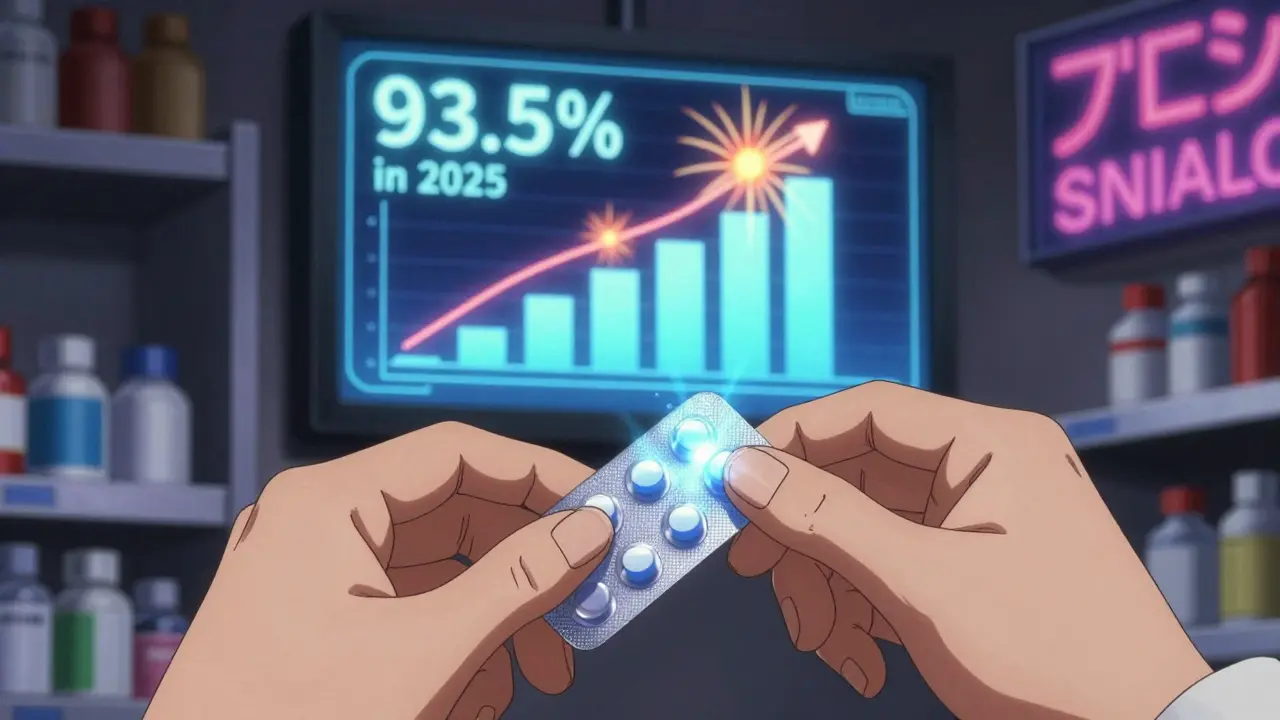
Provider Experience: From Confusion to Confidence
Doctors and nurse practitioners didn’t wake up one day knowing all the rules. It took time. Most need 3 to 6 months to get comfortable with state-specific formularies, PBM requirements, and documentation standards. In states with strong formularies, the process is smooth. In states without, providers spend hours justifying why a brand drug is necessary. That’s time that could be spent treating patients. The shift has also changed prescribing habits. In the past, a doctor might reach for the familiar brand name because it was easier. Now, they’re trained to ask: “Is there a generic? Is it appropriate? Does the patient have a history of reacting poorly?” It’s not about limiting care-it’s about matching the right tool to the job.What’s Next? Biosimilars, Personalized Medicine, and the Future
The next frontier isn’t just generics-it’s biosimilars. These are complex, biologic drugs-like those used for inflammation or nerve pain-that now have generic-like versions. Texas started allowing them in workers’ comp in 2022. More states will follow as patents expire. Looking ahead, pharmacogenomics-the study of how genes affect drug response-is starting to enter the picture. Imagine a worker who has a genetic variation that makes them metabolize certain painkillers slowly. A generic drug might not work as well for them, even if it’s bioequivalent for most people. Testing for these variations could make substitution smarter, not just cheaper. But challenges remain. Specialty drugs-expensive, complex treatments for chronic conditions-now make up 12.7% of workers’ comp pharmacy costs. Yet only 4.3% of those have generic alternatives. That’s where the next cost battle will be fought.
What Workers Should Know
If you’re injured on the job and prescribed a medication, don’t assume the generic is inferior. It’s not. The FDA requires generics to meet the same strict manufacturing standards as brand-name drugs. The same factories often make both. The only difference? Price. If you’re skeptical, ask for the FDA label. Ask your pharmacist to explain bioequivalence. Ask your doctor why they chose that specific drug. Most will be happy to explain. And if you’ve tried a generic and felt no difference? You’re not alone. Eighty-two percent of workers who tried generics reported the same effectiveness as brand-name drugs, according to a 2019 survey.Bottom Line: It’s Not About Cutting Corners-It’s About Cutting Waste
Generic substitution isn’t a cost-cutting gimmick. It’s a smart, science-backed strategy that keeps more money in the system for actual care-physical therapy, surgery, rehabilitation-instead of inflated pill bottles. The data doesn’t lie: higher generic use means lower overall costs, faster recovery times, and no drop in outcomes. The system isn’t perfect. There are gaps, exceptions, and occasional market failures. But the direction is clear. By 2025, generic utilization in workers’ compensation is projected to hit 93.5%. That’s not a prediction-it’s a trajectory. If you’re part of the system, embrace it. If you’re skeptical, educate yourself. And if you’re an injured worker? Trust the science, not the brand name. Your body won’t know the difference-and your wallet will thank you.Are generic drugs really as effective as brand-name drugs in workers’ compensation?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and bioequivalence as their brand-name counterparts. They work the same way in the body. Studies show no difference in clinical outcomes for workers’ compensation patients using generics versus brand-name drugs. The only consistent difference is cost-generics typically cost 80% less.
Can a doctor still prescribe a brand-name drug if a generic is available?
Yes, but only if there’s documented medical necessity. In 38 states with formal drug formularies, including Tennessee and California, the prescribing provider must justify why the brand-name drug is needed-such as a documented allergy, therapeutic failure with the generic, or a narrow therapeutic index. Patient preference alone is not a valid reason.
Why do some workers refuse generic medications?
Many believe brand-name drugs are stronger or higher quality, even though this isn’t true. A 2019 survey found 68% of injured workers initially distrusted generics. But after using them, 82% reported the same effectiveness. Misinformation and marketing from brand-name companies have contributed to this myth. Education from pharmacists and providers helps overcome this barrier.
Do generic drug shortages affect workers’ compensation claims?
Yes. Although rare, shortages do happen-especially for older generics with few manufacturers. When a generic is unavailable, providers may need to prescribe the brand-name version temporarily, or find an alternative. The FDA tracks these shortages, and PBMs adjust formularies in real time to minimize disruption to treatment.
What’s the difference between a generic and a biosimilar?
Generics are exact chemical copies of small-molecule drugs, like painkillers or anti-inflammatories. Biosimilars are highly similar versions of complex biologic drugs-like those used for autoimmune conditions or nerve pain. They’re not identical, but they’re proven to work the same way. The first biosimilars were approved for workers’ comp in Texas in 2022, and more states are adopting them as patents expire.
How do state laws affect generic substitution?
States vary widely. Forty-four states and D.C. allow or require generic substitution where medically appropriate. Some, like Tennessee and California, have strict formularies and require documentation for brand-name use. Others have looser rules, leading to lower generic use. The trend is moving toward mandatory substitution, with Colorado requiring 95% generic use by 2024.
Is there a risk that switching to generics could delay recovery?
No. Multiple studies, including those from the Journal of the American Medical Association and the Workers’ Compensation Research Institute, show no link between generic substitution and slower recovery times. In fact, because generics reduce financial pressure on the system, more resources can be directed toward physical therapy, return-to-work programs, and other recovery supports.

Stacey Smith
December 21, 2025 AT 17:04Generics are cheaper because they don't pay for fancy ads or CEOs' yachts. Same pill. Same results. Stop paying for the logo.
Adrian Thompson
December 22, 2025 AT 23:2490% generics? That's not efficiency, that's a government takeover disguised as cost-cutting. Next they'll be forcing us to take the same insulin as the guy in Nebraska. Who's really profiting here? Not you.
Cameron Hoover
December 24, 2025 AT 14:12It's amazing how science wins when we stop letting fear drive decisions. People think generics are 'lesser'-but the body doesn't care what the bottle looks like. It just wants to heal. And it does.
Theo Newbold
December 25, 2025 AT 02:58Let's be real-PBMs are the real villains. They don't care about your recovery. They care about the rebate they get from the generic manufacturer. The 'savings' are just accounting magic. You're getting the same drug, but now the middleman is richer. The worker? Still in pain.
Grace Rehman
December 26, 2025 AT 14:50What if the real question isn't whether generics work-but why we ever believed the brand name meant better? We've been trained to equate price with value. But the body doesn't read marketing brochures. It responds to chemistry. And chemistry doesn't lie
Orlando Marquez Jr
December 27, 2025 AT 02:05It is of considerable note that the adoption of generic substitution in workers’ compensation systems reflects a broader paradigm shift toward evidence-based pharmaceutical policy. The statistical convergence toward 93.5% utilization by 2025, as corroborated by multiple state-level formulary implementations, suggests a maturation of regulatory frameworks grounded in bioequivalence standards and fiscal prudence.
Jason Silva
December 28, 2025 AT 07:46THEY’RE HIDING SOMETHING. Why do you think the brand-name companies are screaming? Because they know the truth: generics are the ONLY reason workers are getting better faster. They’re not trying to save money-they’re trying to save profits. 💊🔥
Sarah Williams
December 29, 2025 AT 10:40I was skeptical too. Took the generic for my back pain. Same relief. Saved $80. Now I tell every injured coworker: don't judge a pill by its color.
Michael Ochieng
December 30, 2025 AT 00:50Love seeing states like Colorado leading the way. This isn’t just about saving dollars-it’s about redirecting resources to real recovery: PT, mental health, job retraining. Generics are the quiet hero here.
Dan Adkins
December 30, 2025 AT 11:34While the statistical analysis presented herein is commendable, one must consider the macroeconomic implications of pharmaceutical commoditization within the context of global supply chain vulnerabilities. The concentration of active pharmaceutical ingredient manufacturing in foreign jurisdictions introduces systemic risk that is neither addressed nor acknowledged in this discourse.
Erika Putri Aldana
December 30, 2025 AT 20:30so like… the pills are the same but the box is different? lol. why do i feel like im being scammed? 🙄
Jerry Peterson
December 31, 2025 AT 08:53I’ve seen this play out in clinics. Workers panic when they get the generic. But once they realize it works just as well? They’re the ones asking for it next time. It’s a mindset shift, not a medical one.
Southern NH Pagan Pride
December 31, 2025 AT 11:1790% generics? That's the FDA and big pharma working together to control the masses. They don't want you to know that the real meds are kept for the rich. The 'bioequivalent' label? A lie. The fillers are different. The absorption is different. They're poisoning us slowly.
Jackie Be
January 2, 2026 AT 10:09OMG I tried the generic and it actually worked?? I thought I was gonna die 😭 but nope just saved $75 and still feel fine 🙌
John Hay
January 4, 2026 AT 07:51My boss tried to force me to switch to generic. I said no. Now I'm on disability. You think this is about savings? It's about control. They don't care if you heal-they care if you go back to work cheap.