Feeling like the room is spinning? Or just unsteady, lightheaded, or off-balance? You’re not alone. About one in three people over 65 deal with some kind of balance problem, and vertigo is the most common culprit. But here’s the catch: most people think it’s just dizziness - and that’s where things go wrong.
What Exactly Is Vertigo?
Vertigo isn’t just feeling dizzy. It’s the false sensation that you or your surroundings are spinning, tilting, or moving - even when you’re perfectly still. You might feel like you’re on a boat in calm water, or like the walls are swirling around you. It often comes with nausea, vomiting, sweating, or trouble focusing. It’s not the same as lightheadedness, which feels more like you might faint. Vertigo is your inner ear screaming that something’s wrong with your balance system. This isn’t just a nuisance. It can make walking, driving, or even getting out of bed dangerous. The good news? Most cases aren’t caused by something serious - and they can be fixed.The Inner Ear: Your Body’s Balance Center
Your inner ear isn’t just for hearing. It’s packed with tiny tubes and chambers filled with fluid and hair cells that detect movement. Inside those chambers are microscopic calcium crystals called otoconia. Normally, they sit neatly in one spot, helping your brain sense gravity and head position. But sometimes, these crystals get loose. When they drift into the wrong canal - usually the posterior semicircular canal - even a quick head turn, rolling over in bed, or looking up can trigger a spinning sensation. This is called benign paroxysmal positional vertigo (BPPV). It’s the #1 cause of vertigo, making up 20-30% of all dizziness cases, and over half of cases in older adults. Other inner ear problems include:- Vestibular neuritis: A viral infection that inflames the balance nerve. It causes sudden, intense vertigo that lasts days, sometimes weeks - but no hearing loss.
- Meniere’s disease: A fluid pressure disorder in the inner ear. It brings vertigo attacks lasting 20 minutes to hours, along with ringing in the ear (tinnitus), muffled hearing, and that full, plugged-up feeling.
Central Vertigo: When the Brain Is the Problem
About 20% of vertigo cases come from the brain - not the ear. This is called central vertigo. The most common cause? Vestibular migraine. You might not even have a headache. Just dizziness, nausea, light sensitivity, or visual disturbances that last minutes to days. It’s often misdiagnosed as anxiety or inner ear issues. Other brain-related causes - like stroke, multiple sclerosis, or tumors - are rare, but serious. That’s why any new, prolonged vertigo (especially with slurred speech, double vision, weakness, or numbness) needs immediate evaluation. The HINTS exam, used in ERs, can spot stroke with 96.8% accuracy if done within 48 hours.Diagnosis: The Right Test Makes All the Difference
Most doctors won’t test for BPPV unless they’re trained to. That’s why so many people wait weeks - or months - before getting the right diagnosis. A simple test called the Dix-Hallpike maneuver can confirm BPPV in seconds. The doctor turns your head and quickly lays you back. If you feel spinning and your eyes jerk in a specific way, it’s BPPV. For Meniere’s, it’s about tracking symptoms: how long attacks last, whether hearing changes, and if tinnitus is present. For vestibular migraine, keeping a headache and vertigo diary helps spot triggers like stress, sleep loss, or certain foods.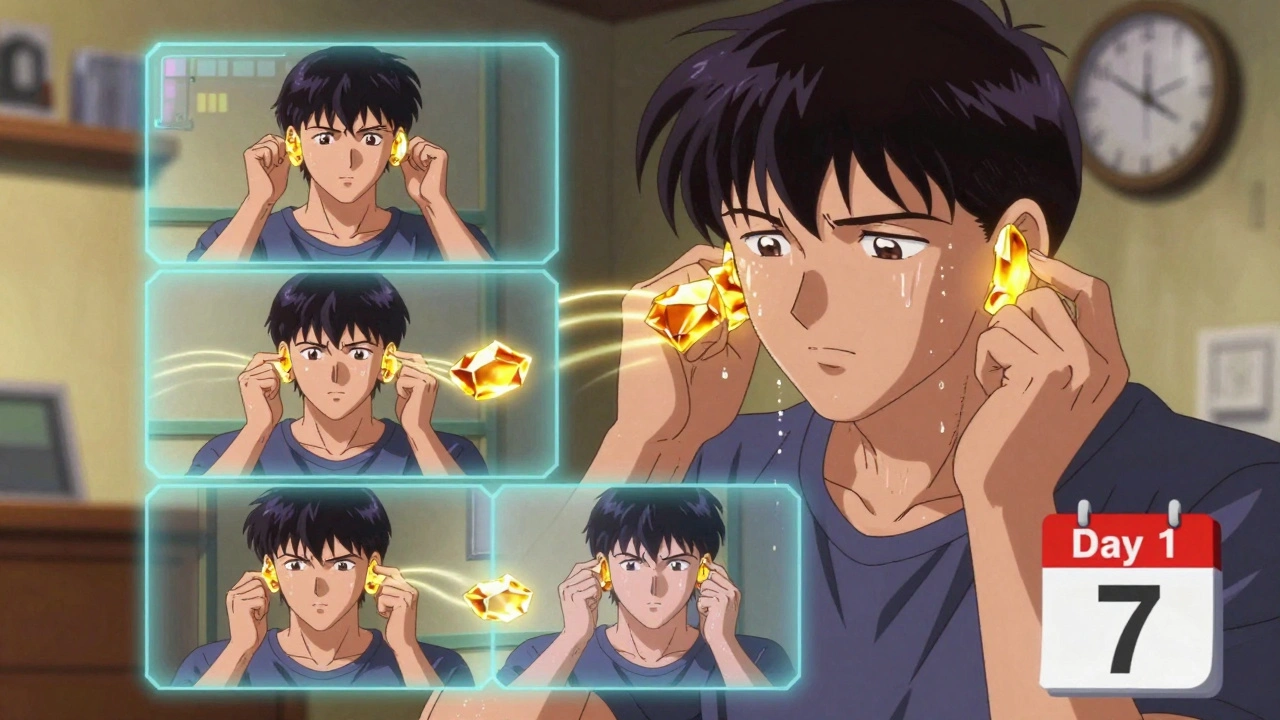
Treatment: Fix the Cause, Not Just the Symptoms
Medications like meclizine (Antivert) or promethazine can help with nausea during a bad attack. But here’s the truth: they don’t cure anything. In fact, taking them longer than 72 hours can slow your brain’s natural ability to adapt - called vestibular compensation. That means you might stay dizzy longer than you need to. The real fix? Targeted therapy based on the cause.BPPV: The Epley Maneuver
The Epley maneuver is a series of head positions designed to move those loose crystals back where they belong. Done correctly, it works in 80-90% of cases after one or two sessions. You can do it at home with video guides - but only if you’ve been properly diagnosed. Doing it when you don’t have BPPV? It won’t help. And doing it wrong? It might make things worse.Meniere’s Disease: Diet and Diuretics
Salt is the enemy. Meniere’s is tied to fluid buildup in the inner ear. Cutting sodium to 1,500-2,000 mg per day - which means avoiding processed foods, canned soups, and restaurant meals - reduces vertigo attacks by 50-70% in most people. Doctors often add a water pill (like triamterene-hydrochlorothiazide) to help flush excess fluid.Vestibular Rehabilitation Therapy (VRT)
This is the most powerful tool for long-term recovery. VRT is physical therapy for your balance system. It’s not about strength - it’s about retraining your brain to rely on other signals (like vision and body sensation) when your inner ear isn’t sending clear messages. Exercises include:- Gaze stabilization: Keeping your eyes focused on a target while moving your head.
- Balance retraining: Standing on one foot, walking heel-to-toe, or standing on foam.
- Habituation: Repeatedly doing movements that trigger dizziness until your brain stops reacting.
Vestibular Migraine: Prevention Over Rescue
You can’t treat a migraine attack with an anti-vertigo pill. Prevention is key. Medications like propranolol, verapamil, or topiramate reduce vertigo frequency by half in 50-60% of patients. New drugs like eptinezumab (Vyepti) are now FDA-approved specifically for vestibular migraine. Tracking triggers - like caffeine, chocolate, lack of sleep, or stress - cuts attacks by 80% in compliant patients.Why Most People Stay Dizzy Longer Than They Should
The biggest reason? Misdiagnosis. One study found 68% of vertigo patients get the wrong diagnosis at least once. BPPV is mistaken for anxiety. Vestibular migraine gets labeled as “just stress.” Meniere’s is ignored until hearing loss gets worse. Another reason? Fear of movement. People stop turning their head, avoid stairs, skip exercise - thinking it’ll prevent attacks. But inactivity makes your balance system weaker. That’s why dizziness gets worse over time. And then there’s medication dependency. Taking meclizine for weeks because “it helps” sounds smart - until you realize you’re not getting better. You’re just numbing the symptoms while your brain loses its chance to heal.What Works - And What Doesn’t
| Treatment | Works For | Effectiveness | Downsides |
|---|---|---|---|
| Epley maneuver | BPPV | 80-95% after 1-3 sessions | Must be done correctly; not for non-BPPV |
| Vestibular rehab therapy | BPPV, vestibular neuritis, Meniere’s, post-stroke | 70-80% improvement in 4-6 weeks | Requires daily effort; initial worsening |
| Sodium restriction (1500-2000mg/day) | Meniere’s disease | 50-70% fewer attacks | Hard to maintain; 75% of sodium comes from processed food |
| Meclizine (Antivert) | Acute vertigo attacks | 70% symptom relief | Causes drowsiness; delays recovery if used >72 hours |
| Bed rest | General dizziness | Minimal benefit | Worsens long-term balance |
Real Stories, Real Results
One woman spent three months being told her vertigo was anxiety. She finally saw an ENT who did the Dix-Hallpike test. The Epley maneuver took 15 minutes. She hasn’t had a spell since. A man with Meniere’s cut out salt, started VRT, and reduced his attacks from daily to once a month. “I thought I’d never drive again,” he said. “Now I drive to work.” A Reddit user posted: “Meclizine made me useless. The Brandt-Daroff exercises took 3 weeks of daily practice. But now? I’m back to hiking.”What to Do Next
If you’re dizzy or spinning:- Don’t panic - most causes are treatable.
- See a doctor who specializes in balance disorders - an ENT or vestibular therapist.
- Ask: “Could this be BPPV? Can you do the Dix-Hallpike test?”
- If it’s BPPV, get the Epley maneuver - don’t wait.
- If symptoms last more than 48 hours, ask about vestibular rehab.
- Stop taking dizziness pills after 3 days unless directed otherwise.
- Track triggers: sleep, stress, salt, caffeine, screen time.
Final Thought
Vertigo isn’t something you just have to live with. It’s not aging. It’s not stress. It’s a signal - your body telling you something’s out of sync. And with the right diagnosis and treatment, most people get back to normal - fast. The key isn’t more pills. It’s understanding what’s wrong, and then doing the work to fix it.Is vertigo the same as dizziness?
No. Dizziness is a broad term that includes lightheadedness, unsteadiness, or feeling faint. Vertigo is a specific type of dizziness - it’s the false sensation that you or your surroundings are spinning. It’s caused by inner ear problems or brain signals gone wrong.
Can I do the Epley maneuver at home?
Yes - but only if you’ve been diagnosed with BPPV by a professional. Doing it without confirmation won’t help and could make symptoms worse. Use a video guide from a trusted source like the Mayo Clinic or Vestibular Disorders Association. Do it slowly, hold each position for 30 seconds, and avoid quick head movements afterward.
How long does vestibular therapy take to work?
Most people notice improvement within 2-4 weeks of daily exercises. Significant progress usually happens by 4-6 weeks. But it requires consistency - twice a day, 5-7 days a week. The first week may feel worse, but that’s part of the process. People who stick with it have an 80-95% success rate.
Why do I feel worse after starting vestibular rehab?
Your brain is relearning how to interpret balance signals. When you move your head in ways that trigger dizziness, it’s forcing your brain to adapt. This causes temporary discomfort - like muscle soreness after starting a new workout. It doesn’t mean you’re hurting yourself. It means the therapy is working. Most people adapt within 7-14 days.
Can vertigo come back after treatment?
Yes, especially with BPPV - recurrence rates are around 15-50% over five years. That’s why it’s important to know the signs and have a plan. If vertigo returns, repeat the Epley maneuver. For Meniere’s or vestibular migraine, long-term management (diet, stress control, medication) helps prevent flare-ups. Regular balance exercises also reduce recurrence risk.
Are there any new treatments for vertigo?
Yes. In 2020, the FDA approved eptinezumab (Vyepti) for vestibular migraine. Smartphone apps like VEDA and VertiGo now help screen for BPPV with 85% accuracy. Researchers are testing drugs that stabilize inner ear crystals to prevent BPPV recurrence. Gene therapy for Meniere’s is in early trials. But the most effective tool remains vestibular rehab - proven for over 30 years.

Heidi Thomas
December 5, 2025 AT 07:34Stop taking meclizine after 3 days. That’s it. No excuses. You’re just numbing the problem and your brain forgets how to fix itself. I’ve seen it a hundred times. People think meds are magic. They’re not. They’re bandages on a broken leg.
Alex Piddington
December 5, 2025 AT 15:02Thank you for this comprehensive overview. It’s refreshing to see such a well-researched piece on vestibular disorders. Many patients are misdiagnosed due to a lack of specialized training among general practitioners. Vestibular rehabilitation therapy remains one of the most underutilized yet effective interventions available.
Libby Rees
December 6, 2025 AT 00:21I’ve had BPPV twice. The first time I waited six months because I thought it was stress. The second time I went straight to the ENT. Dix-Hallpike took 30 seconds. Epley maneuver took five minutes. I’ve been fine for two years. Don’t wait. Get tested.
Dematteo Lasonya
December 7, 2025 AT 20:50This is so helpful. I’ve been dizzy for months and everyone told me to relax. Turns out it was BPPV. I did the Epley at home with a YouTube video and it worked. I cried. Not because it hurt. Because I finally felt like myself again.
Rudy Van den Boogaert
December 8, 2025 AT 05:40I’m not a doctor but I’ve done VRT for vestibular neuritis. First week was brutal. Felt like I was drunk every day. But by week three I could walk without holding the wall. Now I hike. Just keep going. It gets better. Seriously.
Gillian Watson
December 9, 2025 AT 12:37My mum had Meniere’s. Cut salt like crazy. No canned food. No soy sauce. No chips. She said it was torture but after three months her attacks dropped from daily to once a month. She still does balance exercises every morning. No meds. Just discipline.
Pavan Kankala
December 11, 2025 AT 00:55Who really benefits from all this? Pharma. They sell you pills that make you sleepy and then charge you thousands for 'therapy' that's just head tilts. The real cause? Electromagnetic pollution from 5G towers messing with your inner ear crystals. They don't want you to know that.
Martyn Stuart
December 13, 2025 AT 00:01Important note: The Epley maneuver must be performed with the head turned 45 degrees toward the affected side, held for 30 seconds in each position, and followed by 48 hours of avoiding supine positions. Many online videos get this wrong. Always confirm diagnosis with a trained vestibular specialist first.
Jessica Baydowicz
December 14, 2025 AT 13:01YESSSS. I was stuck in a dizziness hell for a year. Thought I was losing my mind. Then I found a vestibular therapist who made me do dumb head moves every day. Felt like a robot. But now? I’m dancing in my kitchen again. No pills. No magic. Just stubbornness and science. You got this!
Shofner Lehto
December 15, 2025 AT 07:48One thing nobody talks about: the emotional toll. Dizziness makes you feel weak. Like you’re failing at being an adult. I hid it for months. Then I realized: this isn’t weakness. It’s biology. And biology can be fixed. VRT didn’t just fix my balance. It fixed my self-worth.
Jake Deeds
December 15, 2025 AT 21:11How ironic that the medical establishment spends billions on drugs while ignoring the simplest, oldest, and most effective treatment: movement. We’ve turned human physiology into a pharmaceutical product. VRT is free. It’s ancient. And it works. But it doesn’t make anyone rich. So they keep you dizzy.
val kendra
December 17, 2025 AT 07:32My daughter had vestibular migraine. We tried everything. Then we tracked her sleep and caffeine. Turns out she was drinking 3 energy drinks a day. Cut it to one. Then none. Attacks dropped 90%. No pills. Just awareness. Sometimes the fix is right under your nose.
Isabelle Bujold
December 18, 2025 AT 00:45I’ve been a vestibular therapist for 18 years. I’ve seen thousands of patients. The most common mistake? Waiting. People think, ‘It’ll go away.’ Or ‘It’s just getting older.’ Or ‘I’ll start VRT next week.’ But the longer you wait, the more your brain forgets how to recalibrate. The nervous system is plastic, yes-but only if you use it. Delaying therapy is like letting a sprained ankle turn into a chronic limp. It’s not just about the ear. It’s about your brain’s ability to adapt. And adaptation has a window. Miss it, and you’re stuck in a cycle of compensation that’s harder to reverse. Do the exercises. Even when it’s hard. Even when you’re scared. Even when you feel like quitting. The first week is the hardest. But the second week? You start to notice small wins. Standing without holding the counter. Walking to the mailbox without nausea. Turning your head without the room spinning. Those are the moments that keep you going. And they’re worth every second of discomfort. You’re not broken. You’re just out of sync. And sync can be restored.