Every year, millions of people in the U.S. and UK take SSRIs to manage depression, anxiety, or OCD. These medications-like sertraline, escitalopram, and fluoxetine-are generally safe and effective. But there’s a hidden danger many don’t know about: serotonin syndrome. It’s not rare. It’s not theoretical. And it’s often triggered by something as simple as adding a common painkiller or herbal supplement to your routine.
What Exactly Is Serotonin Syndrome?
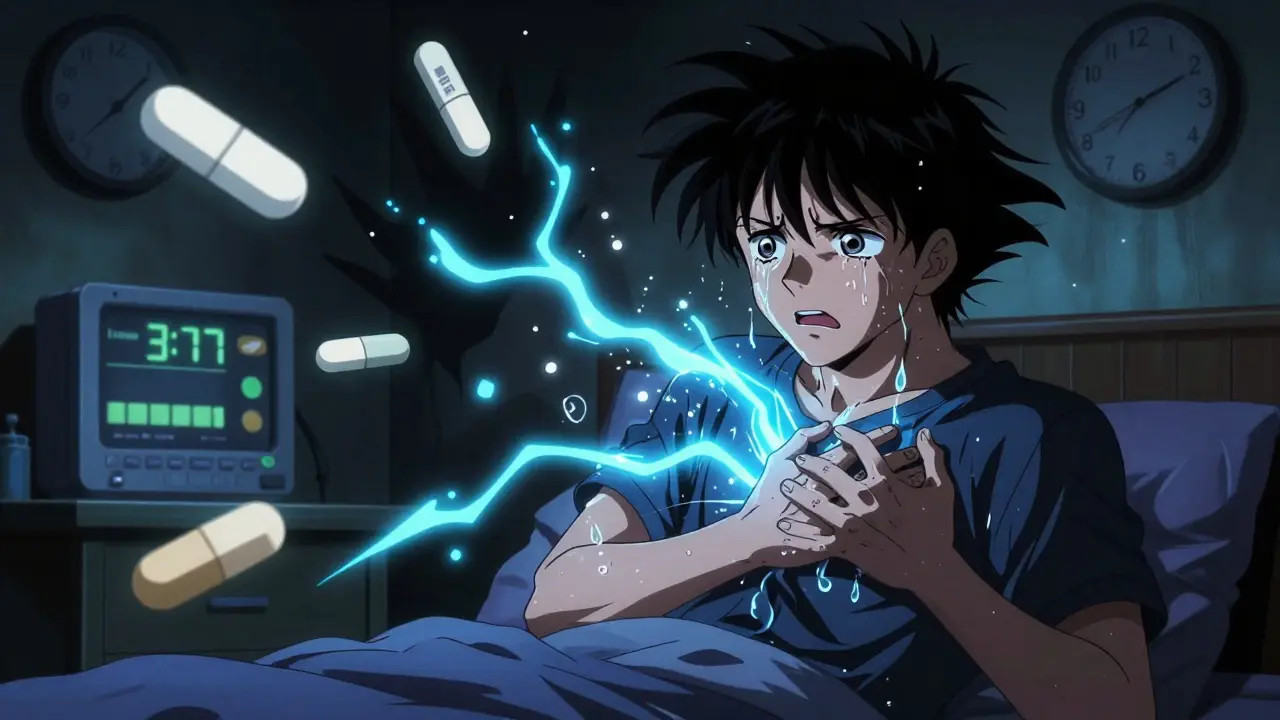
Serotonin syndrome isn’t just "feeling a bit off." It’s a medical emergency caused by too much serotonin building up in your brain and nervous system. Think of serotonin like a neurotransmitter traffic light: normally, it turns on and off smoothly. But when you mix certain drugs, the light stays stuck on green-overstimulating your nerves. Symptoms show up fast-sometimes within hours. You might start shivering uncontrollably, sweating like you’ve run a marathon in winter, or feel your muscles turn rigid. Your heart rate spikes, your temperature climbs past 102°F, and you could become confused, agitated, or even have seizures. In severe cases, it leads to organ failure and death. The Hunter Criteria, now the gold standard for diagnosis, says you have serotonin syndrome if you have one of these: spontaneous muscle twitches (clonus), plus fever and sweating; or muscle stiffness, fever, and eye twitching. If you’re on an SSRI and suddenly feel this way after starting a new medication, don’t wait. Go to the ER.Which Medications Are Most Dangerous When Mixed With SSRIs?
Not all drug combinations are equal. Some are risky. Others are deadly. MAOIs (like phenelzine or selegiline) are the worst. Mixing them with SSRIs is absolutely forbidden. The risk of death is 30-50%. This isn’t a "be careful" warning-it’s a "never do this" rule. Even if you stopped your MAOI two weeks ago, fluoxetine can still be in your system for up to three weeks. That’s why doctors require a five-week washout period if you’re switching from Prozac to an MAOI. Linezolid, an antibiotic used for stubborn infections, is another silent killer. It’s not an antidepressant, but it blocks serotonin breakdown like an MAOI. A 2022 JAMA study found patients over 65 taking linezolid with an SSRI had nearly three times the risk of serotonin syndrome. Many patients don’t realize they’re at risk because linezolid is given for a short course-just 7-14 days. Tramadol, dextromethorphan, and pethidine are opioids, but they act like serotonin boosters. Tramadol alone increases serotonin levels. When combined with sertraline or fluoxetine, the risk jumps 4.7 times. A Reddit user described being hospitalized after taking tramadol for back pain while on sertraline: "Within 12 hours, I was burning up, shaking, and couldn’t move my legs. The ER doctor said I was lucky I didn’t have a seizure." SNRIs like venlafaxine or duloxetine are also antidepressants, but they increase both serotonin and norepinephrine. Combining them with SSRIs triples the risk of serotonin syndrome. Yet, doctors still prescribe this combo-often to treat treatment-resistant depression-without warning patients. St. John’s wort, the herbal supplement many take for mild depression, is just as dangerous. One user on Drugs.com wrote: "I took St. John’s wort with my Prozac for three days. I started shaking, couldn’t think straight, and thought I was losing my mind. The ER said it was serotonin syndrome." The FDA has warned about this for years. Still, people buy it online thinking it’s "natural" and therefore safe.What About Other Opioids? Are Some Safer?
Not all painkillers are created equal. If you’re on an SSRI and need pain relief, your options matter. High-risk opioids: tramadol, dextromethorphan, pethidine. Avoid them completely. Medium-risk: methadone, fentanyl. Use only under close supervision. Low-risk: morphine, codeine, oxycodone, buprenorphine. These don’t significantly raise serotonin levels. A 2023 FDA review found no meaningful increase in serotonin syndrome risk with these when taken with SSRIs. The CDC now explicitly recommends choosing morphine or oxycodone over tramadol for patients on SSRIs. Many primary care doctors still default to tramadol because it’s cheaper and doesn’t require special prescriptions. That’s changing-but slowly.
Who’s Most at Risk?
It’s not just about what you take-it’s who you are. People over 65 are at highest risk. One in five Americans in that age group takes an SSRI. One in five also takes an opioid. Nearly 22% take five or more medications daily. That’s a perfect storm for interactions. Pharmacists in the UK and U.S. report a 40% rise in serotonin syndrome cases among elderly patients since 2020. People with genetic differences in liver enzymes (CYP2D6 poor metabolizers) are also more vulnerable. If your body can’t break down tramadol properly, even a normal dose can flood your system with serotonin. Genetic testing isn’t routine-but if you’ve had bad reactions to meds before, it’s worth asking your doctor about. And then there’s the problem of polypharmacy. Many patients see multiple specialists-a psychiatrist, a pain doctor, a cardiologist-each prescribing something new. No one connects the dots. A 2023 study found pharmacist-led medication reviews cut serotonin syndrome events by 47%. That’s not luck. That’s system change.What Should You Do If You’re on an SSRI?
You don’t need to stop your medication. But you need to be smarter.- Know your meds. Make a list-prescription, over-the-counter, supplements. Bring it to every appointment.
- Ask your pharmacist. They’re trained to spot interactions. Don’t assume your doctor knows every drug you’re taking.
- Watch for the 5 S’s: Shivering, Sweating, Stiffness, Seizures (rare), Sudden confusion. If you notice any of these after starting a new drug, stop it and call your doctor-or go to urgent care.
- Never start St. John’s wort, tryptophan, or 5-HTP. These are not "natural" alternatives. They’re serotonin boosters. And they’re dangerous with SSRIs.
- Be extra careful after dose changes. Increasing your SSRI or adding a new drug is when most cases happen.

How Is This Being Fixed?
The system is waking up. In 2024, the FDA mandated that all electronic prescribing systems must include real-time alerts for high-risk combinations-like SSRI + tramadol or SSRI + linezolid. Hospitals using Epic, Cerner, and other platforms have already seen a 32% drop in dangerous co-prescriptions. In the UK, the National Poisons Information Service reports that serotonin syndrome is now the most common cause of death from antidepressant overdose. They’ve trained ER staff to recognize it faster. In the U.S., the CDC updated its opioid prescribing guidelines to push doctors toward safer alternatives. There’s even a new blood test in development-SerotoninQuant-that could confirm serotonin syndrome with a simple lab draw. It’s still in trials, but if it works, it could end years of misdiagnosis.Bottom Line: You’re Not Overreacting If You’re Worried
SSRIs save lives. But they’re not harmless. The risk of serotonin syndrome is small-about 1 in 1,000 people per year. But when it happens, it can kill you in hours. You don’t need to fear your medication. You need to respect it. Talk to your doctor. Know what you’re taking. Ask about interactions. Don’t let a simple painkiller or herbal tea become your worst mistake. If you’re on an SSRI and your doctor suggests a new drug-especially an opioid, antibiotic, or supplement-ask: "Could this cause serotonin syndrome?" If they hesitate, get a second opinion. Your life might depend on it.Can serotonin syndrome happen with just one SSRI?
Rarely. Serotonin syndrome almost always occurs when an SSRI is combined with another serotonergic drug. Taking an SSRI alone at the correct dose is very unlikely to cause it. Most cases involve adding a new medication-like tramadol, St. John’s wort, or an MAOI.
How long does it take for serotonin syndrome to develop?
Symptoms usually appear within hours of taking a new drug, often within 2-6 hours. In some cases, they can start within 30 minutes. If you’ve just started a new medication and feel suddenly unwell-shivering, sweating, stiff muscles-don’t wait. Seek help immediately.
Is serotonin syndrome the same as an SSRI overdose?
No. An overdose means you took too much of one drug. Serotonin syndrome is about drug interactions-even at normal doses. You can develop it by taking your regular SSRI plus one extra pill of tramadol. It’s not about quantity-it’s about combination.
Can I take ibuprofen or acetaminophen with an SSRI?
Yes. Ibuprofen and acetaminophen (Tylenol) do not affect serotonin levels and are considered safe with SSRIs. They’re the preferred pain relievers if you’re on an SSRI and need something for headaches or muscle pain.
What should I do if I think I have serotonin syndrome?
Stop taking all new medications immediately. Go to the nearest emergency room. Tell them you’re on an SSRI and suspect serotonin syndrome. Do not wait to see your doctor. This is a medical emergency. Treatment includes stopping the triggering drugs, giving IV fluids, and sometimes medications like cyproheptadine to block serotonin.
Are there any long-term effects after recovering from serotonin syndrome?
Most people recover fully within 24-72 hours with proper treatment. However, severe cases can cause lasting nerve damage or muscle injury. Some patients report lingering anxiety or sensitivity to medications afterward. Always follow up with your doctor after an episode to review your medication list and avoid future risks.
Napoleon Huere
January 25, 2026 AT 08:23It’s wild how we treat brain chemistry like a faucet you can just turn up without consequences. We’ve got people popping SSRIs like candy while throwing in St. John’s wort because it’s ‘natural’-like that makes it safe. Serotonin isn’t some mystical life force. It’s a molecule. Too much of it and your nervous system goes full meltdown mode. The fact that ERs are seeing more of this now isn’t a coincidence-it’s the result of a medical culture that treats drugs like snacks.
Shweta Deshpande
January 25, 2026 AT 18:01OMG I’m so glad someone finally wrote this!! 🙌 I had a cousin who went to the hospital after mixing sertraline with that herbal tea she swore was ‘calming’-turns out it was St. John’s wort. She was shaking so bad she couldn’t hold her coffee cup, and she thought it was just ‘anxiety.’ We all thought it was fine because it was ‘natural.’ But nope. Her body went rogue. Now she’s on a strict meds list and sees a pharmacist every time she gets a new prescription. Knowledge is power, y’all! 💪
Aishah Bango
January 27, 2026 AT 17:55If you’re dumb enough to mix SSRIs with random supplements you bought off Amazon, you deserve what you get. This isn’t rocket science. It’s basic biology. People treat their brains like a video game where you can just spam power-ups. Wake up. Your body isn’t a sandbox. One wrong move and you’re in the ER. No sympathy.
Simran Kaur
January 28, 2026 AT 09:08As someone from India where herbal remedies are part of daily life, I’ve seen this happen too many times. My auntie took ashwagandha with her fluoxetine because her neighbor said it ‘helps with stress.’ Three days later, she was in the ICU-shaking, fever, confused. The doctors said it was serotonin syndrome. She didn’t even know what that meant. We need better education-not just in the West, but everywhere. In my village, people trust Grandma’s advice more than a doctor’s. That’s dangerous when it comes to brain chemistry. 🙏 Let’s spread awareness gently but firmly.
Neil Thorogood
January 29, 2026 AT 16:24Tramadol with SSRIs? 😳 Bro, that’s like putting a lit match next to a gas can labeled ‘DO NOT TOUCH.’ And yet, doctors still prescribe it like it’s Advil. I’m not even mad-I’m just impressed at how efficiently we’ve turned healthcare into a Russian roulette game. 🎰 #PharmaceuticalRussianRoulette #StopWithTheTramadol
Jessica Knuteson
January 30, 2026 AT 06:36Robin Van Emous
February 1, 2026 AT 02:24I just want to say thank you for writing this. I’ve been on sertraline for 8 years and never knew about the linezolid risk. My dad had to take it after knee surgery last year-I didn’t even think to ask if it was safe. I’m going to print this out and bring it to his next appointment. I also told my mom to stop taking that ‘mood booster’ tea she’s been drinking. She didn’t believe me until I showed her the FDA warning. Little things matter. Thank you for being the voice we need.
Angie Thompson
February 2, 2026 AT 09:18Y’all I just had the biggest ‘oh crap’ moment reading this 😳 I’ve been taking ibuprofen with my Lexapro and thought I was golden-but now I’m wondering… did I ever take tramadol for that back pain last winter??!! I’m gonna check my pharmacy log right now. Also-St. John’s wort?? I thought it was like chamomile but for your brain!! 😭 This is why I love Reddit. Someone saves your life without even knowing it. 💙
Karen Droege
February 2, 2026 AT 12:01Let me tell you something-this isn’t just about drugs. It’s about the collapse of medical oversight. Doctors don’t talk to each other. Pharmacists are overworked. Patients are treated like numbers. I’ve seen patients on six antidepressants, three painkillers, and two ‘wellness’ supplements. And then they wonder why they’re hallucinating. This isn’t negligence-it’s systemic failure. We need mandatory interdisciplinary reviews. Not just for the elderly-for everyone. Because your ‘simple’ painkiller? Could be your last.
George Rahn
February 2, 2026 AT 13:15Another liberal panic over pharmaceuticals. People take SSRIs because they’re weak. They take supplements because they’re gullible. And now we’re turning a medical fact into a fear campaign. Serotonin syndrome is rare. The real problem is people who can’t handle their own emotions and medicate themselves into oblivion. Stop blaming the drugs. Start blaming the culture of victimhood.
Ashley Karanja
February 3, 2026 AT 14:14Thank you for this incredibly comprehensive breakdown. As a clinical pharmacist, I’ve seen too many serotonin syndrome cases-especially in polypharmacy elderly patients. The real tragedy? Most were preventable. We’re not talking about rare outliers. We’re talking about predictable, documented, avoidable events. The FDA’s new e-prescribing alerts? Long overdue. But we also need better patient education-plain language, visual aids, maybe even QR codes on pill bottles linking to interaction guides. We can do better. We must.
bella nash
February 5, 2026 AT 00:33SWAPNIL SIDAM
February 6, 2026 AT 10:07Bro I live in India and we have this problem too. People buy antidepressants from local chemists without prescription. Then they add ashwagandha, gotu kola, even turmeric with black pepper. One guy came to our clinic shaking like a leaf-turned out he was on fluoxetine + 5-HTP. We saved him. But he didn’t even know what he was taking. We need to teach people-not scare them. Just… tell them.
Geoff Miskinis
February 7, 2026 AT 01:26How quaint. A 12-page essay on serotonin syndrome as if it’s some novel discovery. In the UK, we’ve known about this since the 1990s. The real issue is the American obsession with self-diagnosis and DIY pharmacology. You don’t need a Reddit post to understand that mixing MAOIs with SSRIs is lethal. You need a basic biology class. Or, you know, a doctor. But apparently, that’s too much to ask.
Sally Dalton
February 7, 2026 AT 01:55thank you thank you thank you!! i had no idea about linezolid!! my mom just finished a 10-day course for pneumonia and she’s on escitalopram… i’m calling her right now to tell her to stop the herbal tea she’s been drinking too 😭 i’m so glad i read this before it was too late. you’re a lifesaver!! 🙏💖