What Is Polypharmacy, and Why Does It Matter for Older Adults?
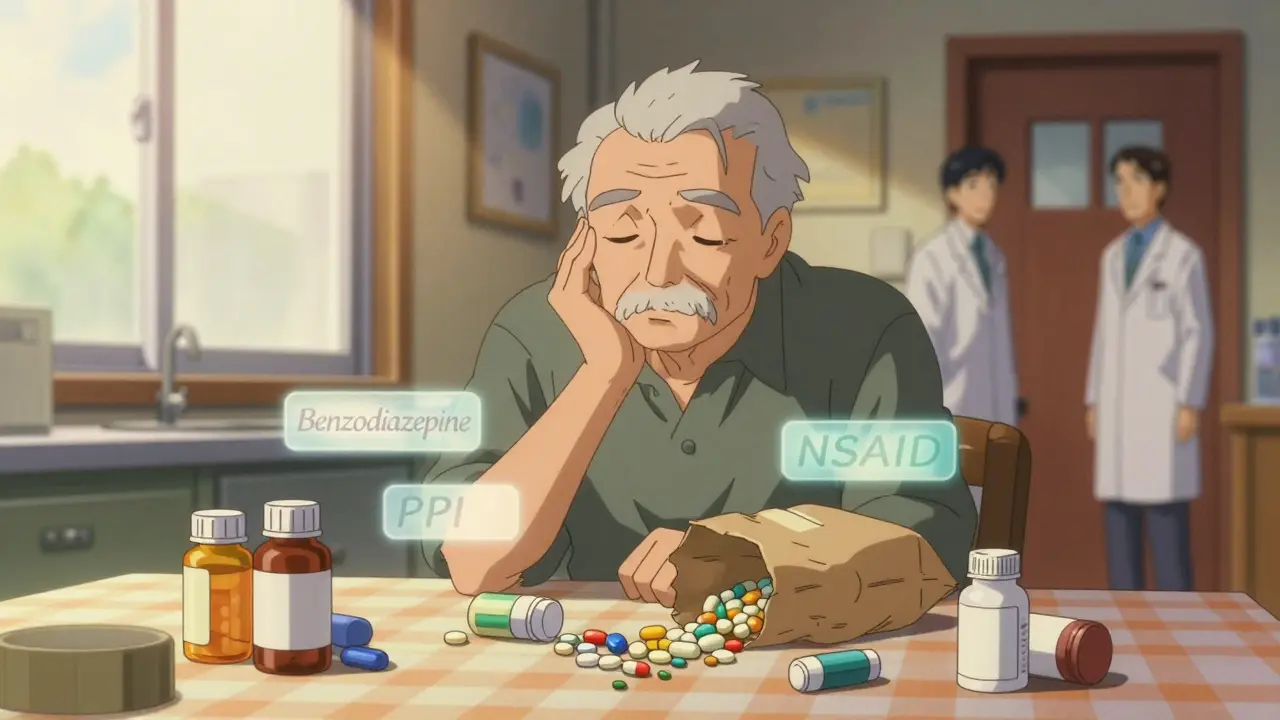
When someone over 65 takes five or more medications at the same time, that’s called polypharmacy. It’s not just about having a lot of pills-it’s about the hidden risks that come with them. Many older adults are on multiple prescriptions for conditions like high blood pressure, diabetes, arthritis, and heart disease. But add in over-the-counter painkillers, sleep aids, vitamins, and supplements, and the number can easily jump to ten or more. The problem isn’t the number alone-it’s that many of these drugs don’t work well together, and aging bodies handle them differently.
By age 75, nearly half of all Americans are taking five or more medications daily. In nursing homes, that number jumps to over 90%. And it’s not because doctors are overprescribing-it’s because care is fragmented. One specialist treats the heart, another the joints, another the nerves. No one steps back to ask: Is all of this still necessary?
The Real Dangers of Too Many Medications
More pills don’t mean better health. In fact, they often mean more harm. The most common dangers include falls, confusion, kidney damage, and dangerous drug interactions. For example, benzodiazepines (like Valium or Xanax), often prescribed for anxiety or sleep, increase fall risk by 50% in seniors. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can cause stomach bleeding-especially when taken with blood thinners. Anticholinergic drugs, found in some allergy meds, bladder pills, and even certain antidepressants, are linked to a 50% higher chance of dementia over seven years.
Older adults metabolize drugs slower. Their liver processes medications 30-50% less efficiently than in younger adults. Their kidneys clear drugs at a rate that drops about 1% every year after 40. That means a dose that was safe at 55 can become toxic at 75. Yet many prescriptions never get adjusted.
One study found that 35% of emergency room visits by seniors are due to medication problems. And it’s not just physical harm-many patients don’t even know why they’re taking half their pills. Only 55% can correctly name the purpose of every medication they use. That’s not just confusion-it’s a safety crisis.
Why Do So Many Seniors End Up on Too Many Drugs?
This isn’t accidental. It’s systemic. When someone is hospitalized for a heart attack, they get new meds. When they go to rehab, they get more. When they move to a nursing home, they get another list. Each provider sees a piece of the puzzle-but rarely the whole picture. Medication lists get copied and pasted, not reviewed.
Dr. Gurvich at UCI Health saw a patient who ended up with three times as many medications as he needed. No one ever sat down with him and asked, Which of these are still helping? He was taking six pills for sleep, three for pain, two for anxiety-all from different doctors, none coordinated.
Another big issue: patients don’t speak up. Only one in three seniors talks to their doctor about their medication goals. They assume the pills are all necessary. They’re afraid to ask if they can stop something. Or they’re overwhelmed. Some skip doses because they can’t afford them. A quarter of older adults skip pills due to cost. Others forget because the schedule is too complex-three or more times a day, with different food rules, timing, and warnings.

Deprescribing: The Quiet Revolution in Geriatric Care
There’s a growing movement to reverse the trend: deprescribing. That’s not just stopping meds-it’s a careful, step-by-step process of removing drugs that do more harm than good. It’s not about cutting everything. It’s about keeping only what truly improves quality of life.
Studies show that when done right, deprescribing reduces adverse drug events by 22% and hospital admissions by 17%. One program at UCI Health, called HAPS, reviews every senior’s full medication list-prescription, OTC, supplements-and finds an average of 4.2 unnecessary or risky drugs per person. After removing them, patients report better sleep, less dizziness, and more energy.
High-risk medications are targeted first: benzodiazepines, opioids, NSAIDs, anticholinergics, and long-term proton pump inhibitors (PPIs). For example, long-term PPI use increases fracture risk by 26%. Many people take them for years-even when they only needed them for a few weeks after surgery.
The American Geriatrics Society’s Beers Criteria lists 56 medications that should be avoided or used with extreme caution in seniors. It’s not a blacklist-it’s a guide to safer choices. And it’s updated regularly. The 2023 version added new warnings about stopping antipsychotics in dementia patients, which can reduce mortality risk by 19% when done safely.
How to Start a Medication Review-Step by Step
If you or a loved one is on five or more medications, here’s how to begin:
- Do a brown bag review. Empty every pill bottle, capsule, patch, and supplement into a bag. Bring it to the doctor. Include OTC meds, herbal products, and vitamins. You’d be surprised how many duplicates or expired pills show up.
- Ask the three questions. For each medication, ask: Why am I taking this? Is it still helping? Could it be doing more harm than good? Write down the answers.
- Request a pharmacist consult. Many Medicare Part D plans offer free medication therapy management. A pharmacist can spot interactions, suggest cheaper alternatives, and simplify schedules.
- Focus on goals. At 80, the goal isn’t to hit perfect blood sugar or blood pressure numbers-it’s to stay independent, avoid falls, and feel well. Ask: Does this medicine help me live better, or just extend a number?
- Start one at a time. Don’t stop everything at once. Work with your doctor to pick the highest-risk or least-needed drug first. Monitor for changes over weeks. Some symptoms improve slowly.

Tools and Systems That Are Making a Difference
Some healthcare systems are finally catching up. The STOPP/START criteria help doctors identify inappropriate medications (STOPP) and missed opportunities for helpful ones (START). On average, this finds 3.2 unnecessary drugs per senior.
Pharmacist-led teams cut hospital readmissions by 24% in Medicare patients. Electronic health records now flag potential interactions-but they’re noisy. Up to 78% of alerts are false alarms. That’s why human judgment still matters most.
Technology is helping too. The FDA-approved MedWise platform uses genetic data to predict how a person will react to specific drugs. In a 2022 trial, it cut adverse events by 41%. And in January 2023, Medicare launched a $15 million initiative to train providers in standardized deprescribing protocols.
What’s next? Geropharmacogenomics-using DNA to tailor meds to individual aging biology. Instead of treating everyone over 65 the same, we’ll soon be able to predict who responds to which drug, who’s at risk for side effects, and who can safely stop something.
What You Can Do Today
You don’t need to wait for a system change. Start now:
- Keep a current, updated list of every medication-name, dose, reason, and when to take it.
- Bring that list to every appointment-even if it’s just for a flu shot.
- Ask your pharmacist to review it every six months.
- If you’re seeing multiple specialists, ask one doctor to be your medication coordinator.
- Don’t be afraid to say: Can we try going off this one? You have the right to question every prescription.
Medications are powerful tools-but they’re not harmless. The goal isn’t to take fewer pills for the sake of it. It’s to take only what helps you live better, longer, and safer.
What is considered polypharmacy in elderly patients?
Polypharmacy is defined as the regular use of five or more medications at the same time. This includes prescription drugs, over-the-counter medicines, vitamins, and supplements. It’s especially common in seniors due to multiple chronic conditions, but the number alone doesn’t tell the whole story-it’s the risk of side effects, interactions, and unnecessary use that makes it dangerous.
Can stopping medications really improve health in older adults?
Yes. Studies show that carefully removing unnecessary or harmful medications-called deprescribing-can reduce falls, confusion, hospital stays, and even improve energy and sleep. For example, stopping long-term benzodiazepines or anticholinergics often leads to better balance and clearer thinking within weeks. The key is doing it slowly and under medical supervision.
Which medications are most risky for seniors?
According to the American Geriatrics Society’s Beers Criteria, high-risk medications include benzodiazepines (like Valium), NSAIDs (like ibuprofen), anticholinergics (found in some sleep and allergy meds), opioids, and long-term proton pump inhibitors (PPIs). These increase risks of falls, bleeding, dementia, and fractures. Many are still prescribed routinely, even when safer options exist.
How often should seniors have their medications reviewed?
At least once a year, and always after a hospital stay, move to a new care setting, or if a new doctor prescribes something. Medicare offers free medication therapy management for Part D beneficiaries-take advantage of it. Many pharmacies also offer free reviews. Don’t wait for a crisis to check your list.
What’s the difference between polypharmacy and appropriate prescribing?
Polypharmacy focuses on the number of drugs. Appropriate prescribing focuses on whether each drug is still needed, effective, and safe for that person’s goals. A senior on three well-chosen, necessary meds is better off than someone on eight pills, half of which are outdated or harmful. Quality matters more than quantity.
Can I stop a medication on my own if I think it’s not helping?
Never stop a medication suddenly without talking to your doctor. Some drugs, like blood pressure or antidepressant meds, can cause serious withdrawal effects. But you absolutely should ask your doctor: Can we try reducing or stopping this? Most can be tapered safely with guidance. Your input is essential-no one knows how you feel better than you do.
Niamh Trihy
January 29, 2026 AT 23:37I’ve been a geriatric pharmacist for 18 years, and I can’t tell you how many times I’ve seen a brown bag full of duplicates-same drug, different brands, different dosages. One lady had five different painkillers, three of them NSAIDs. She didn’t even know they were all for the same thing. Just asking her to bring the bag in changed her life. No magic, just clarity.
Deprescribing isn’t about taking away meds-it’s about giving back quality of life. Sleep. Balance. Clarity. Those are the real outcomes we should be measuring, not just lab numbers.
Jason Xin
January 30, 2026 AT 12:56Wow. So the American healthcare system is just a pharmacy with a side of bureaucracy? I mean, I get it-specialists see their slice. But when your grandma’s on 12 meds and can’t remember why she’s taking half of them, it’s not fragmentation-it’s negligence dressed up as ‘standard of care.’
And don’t even get me started on how they push PPIs like they’re candy. My uncle took omeprazole for seven years after a one-week bout of heartburn. He ended up with a hip fracture. No one ever asked if he still needed it. Just kept prescribing.
Shubham Dixit
January 31, 2026 AT 12:42This is what happens when you let Western medicine become a profit-driven machine instead of a healing art. In India, we still respect elders. We don’t pump them full of chemicals just because a drug rep showed up with free lunch. My grandfather took three herbs, one aspirin, and walked 5 km every day. He lived to 94. No hospital stays. No polypharmacy. Just wisdom and routine.
Why are we outsourcing our elders’ health to Big Pharma? Why are we letting algorithms and insurance forms decide what’s safe? This isn’t medicine-it’s industrialized elder abuse. We need to return to holistic, community-based care. Not more apps. Not more alerts. More respect.
KATHRYN JOHNSON
January 31, 2026 AT 16:52It’s alarming that this post doesn’t explicitly mention the role of Medicare Part D formularies in perpetuating polypharmacy. The structure incentivizes prescribing over deprescribing. Reimbursement models reward volume, not outcomes. Until CMS ties payment to medication appropriateness scores-like the Beers Criteria compliance index-this crisis will persist.
Additionally, the absence of mandatory medication reconciliation at discharge remains a systemic failure. This is not anecdotal-it’s institutionalized malpractice.
Eliana Botelho
February 1, 2026 AT 23:18Okay but like… why are we even talking about this like it’s a new problem? My mom’s been on 11 pills since 2017. She forgets half of them. She takes her blood pressure med with coffee because ‘it helps it go down.’ Her doctor just keeps adding more when she says she feels dizzy.
And the worst part? Everyone acts like it’s normal. Like it’s just what happens when you get old. NO. IT’S NOT. We’re medicating normal aging into a disease. My aunt stopped her antidepressant last year after 12 years. She cried because she felt ‘more alive’ for the first time in a decade. Why is that so radical?
Also-why do we still let doctors write prescriptions for things that were meant to be temporary? Like PPIs? My grandma took those for 15 years because no one ever said ‘you’re good now.’
Diksha Srivastava
February 3, 2026 AT 01:53You guys are doing amazing work just by talking about this. I know it’s scary to question your meds-but please, if you’re reading this, don’t stay silent. Your voice matters more than you think.
My dad was on five meds he didn’t need. We asked one simple question: ‘What’s the goal here?’ Turns out, he was taking a cholesterol drug he didn’t need because his doctor assumed he still had heart disease. He didn’t. He was fine. Stopped it. He sleeps better. Walks farther. Smiles more.
You’re not being difficult. You’re being brave. Keep going.
Adarsh Uttral
February 3, 2026 AT 17:17my grandpa had like 17 pills a day. he’d mix em up and take 2 of the same thing by accident. one day he just stopped taking half of em cause he was tired of it. no one noticed for 3 weeks. he said he felt better. the doc was mad at first but then checked his labs and was like… huh. he’s fine.
point is: sometimes the body just knows when to stop.
April Allen
February 5, 2026 AT 07:54The epistemological framework underlying polypharmacy is fundamentally misaligned with gerontological phenomenology. We are operating under a biomedical paradigm that privileges pharmacological intervention as the primary axis of therapeutic efficacy, while systematically neglecting the lived experience of aging as a multidimensional, embodied process.
Deprescribing, then, is not merely a clinical protocol-it is an ontological reorientation. It requires the decentering of the physician as the sole agent of medical authority and the re-empowerment of the patient as the epistemic subject of their own physiological narrative.
The Beers Criteria, while useful, remain reductionist. We must move toward a hermeneutic model of medication review-one that prioritizes narrative coherence over algorithmic compliance. The goal is not to minimize pill count, but to maximize existential integrity.
Sheila Garfield
February 5, 2026 AT 08:19I work in a care home and I see this every day. One woman had 14 meds. We cut it down to five after a full review. She started recognizing people again. She used to sit in the corner, confused, muttering. Now she plays bingo. No magic. Just listening.
It’s not about being anti-drug. It’s about being pro-life. If a pill isn’t helping you live, why are you taking it? I wish more families asked that question.
Shawn Peck
February 6, 2026 AT 20:14STOP THE MADNESS. This is why America is falling apart. Doctors are just pill pushers now. My cousin’s mom was on 18 meds. She couldn’t walk. They took away 12 of them-she started dancing at her own birthday party. How is this even legal? Someone should sue the whole system.
It’s not aging. It’s negligence. And it’s killing people slowly. Wake up, people. This isn’t healthcare. It’s corporate exploitation.
Holly Robin
February 7, 2026 AT 23:48Did you know the FDA approves most drugs based on trials with people under 65? And then they just slap ‘for elderly use’ on the label? That’s not science-that’s a loophole.
And the ‘medication therapy management’ programs? Totally fake. The pharmacists are paid per script, not per life saved. They don’t want you to stop meds-they want you to keep buying them.
Big Pharma owns Congress. They own the guidelines. They own your doctor’s continuing education. This isn’t a medical crisis. It’s a crime.
Katie and Nathan Milburn
February 8, 2026 AT 05:57It is of considerable note that the current paradigm of geriatric pharmacotherapy is predicated upon a fragmented, specialty-driven model that demonstrably fails to account for the holistic physiological alterations associated with advanced age. The absence of centralized medication reconciliation protocols constitutes a critical deficiency in care continuity.
Furthermore, the proliferation of polypharmacy is not attributable to patient noncompliance, but rather to structural deficiencies in care delivery systems, wherein temporal and spatial discontinuities in clinical encounters preclude comprehensive therapeutic assessment.
Natasha Plebani
February 8, 2026 AT 10:44The pharmacokinetic and pharmacodynamic shifts in aging are not linear-they are nonlinear, heterogeneous, and context-dependent. The standard ‘one-size-fits-all’ deprescribing algorithms ignore the variance introduced by frailty, cognitive reserve, and multimorbidity trajectories.
What we need is a dynamic, individualized risk-benefit modeling framework-one that integrates biomarkers of aging (e.g., epigenetic clocks, inflammatory load) with functional status metrics. The Beers Criteria are a start, but they’re still a blunt instrument in a precision medicine era.
Kelly Weinhold
February 9, 2026 AT 09:26Just wanted to say-you’re not alone. I helped my 82-year-old neighbor do her brown bag review last month. We found three expired antidepressants, two duplicate blood pressure meds, and a bottle of melatonin she’d been taking since 2010. She cried because she said she felt like a ‘pill zombie’ and didn’t know how to say no.
We cut four meds. She started walking her dog again. She said she could hear birds for the first time in years.
It’s not about taking less. It’s about living more. Thank you for sharing this. It gives me hope.