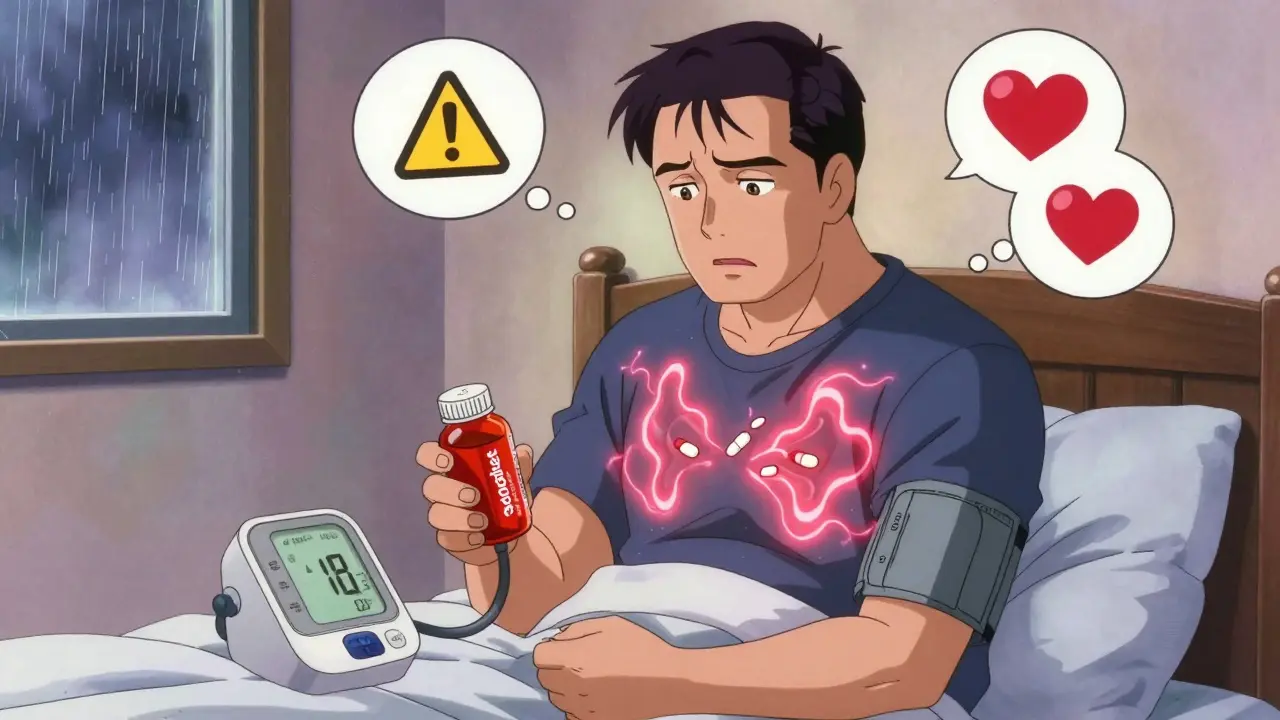
If you're on blood pressure medication and get a stuffy nose, you might reach for a nasal decongestant without thinking twice. But that simple cold remedy could be putting your heart at risk. Nasal decongestants aren't harmless over-the-counter fixes-they can spike your blood pressure, undo the work of your prescription drugs, and even trigger dangerous heart events. This isn't theoretical. Every year, thousands of people with high blood pressure end up in emergency rooms because they didn't realize their cold medicine was making their condition worse.
How Nasal Decongestants Raise Blood Pressure
Nasal decongestants like pseudoephedrine and phenylephrine work by tightening blood vessels in your nose. That reduces swelling and lets you breathe easier. But here’s the catch: they don’t just tighten vessels in your nose. They tighten them everywhere-in your arms, legs, kidneys, and heart. This forces your heart to pump harder to push blood through narrower pathways. The result? Your blood pressure rises.It doesn’t take much. A single dose of pseudoephedrine can bump systolic blood pressure up by 5 to 10 mmHg. For someone with well-controlled hypertension, that might seem small. But for someone on the edge, or taking multiple blood pressure meds, that spike can be enough to trigger chest pain, irregular heartbeat, or even a stroke. The effect is stronger with immediate-release formulas and higher doses. Even topical sprays like oxymetazoline (Afrin) can get into your bloodstream and cause the same problem-something most people don’t realize.
Which Decongestants Are the Most Dangerous?
Not all decongestants are created equal. The biggest red flags are:- Pseudoephedrine - Found in Sudafed and many multi-symptom cold formulas. It’s the most potent and most likely to cause problems.
- Phenylephrine - Now the most common decongestant in OTC products after pseudoephedrine was moved behind the counter. Still risky. A 2005 study showed it raises blood pressure, especially in higher doses.
- Ephedrine - Rare in the U.S. now, but still found in some herbal supplements. Extremely dangerous for people with heart conditions.
- Oxymetazoline - The active ingredient in Afrin and other nasal sprays. People think topical = safe. It’s not. It can still enter your bloodstream.
And here’s the sneaky part: you won’t always see these names clearly labeled. In combination cold and flu products, decongestants are often buried in a long list of ingredients. Look for “decongestant,” “sinus relief,” or “congestion” on the front-but always check the Active Ingredients section on the back.
How Decongestants Interfere With Blood Pressure Meds
Your blood pressure medications are carefully balanced to keep your numbers stable. Decongestants throw that balance off in several ways:- Beta-blockers (like metoprolol): Decongestants can counteract their effects by increasing heart rate and forcing the heart to work harder, making the drug less effective.
- Calcium channel blockers (like nifedipine or felodipine): These relax blood vessels. Decongestants do the opposite-tightening them. The two fight each other, leading to unpredictable pressure spikes.
- ACE inhibitors and ARBs: These help your body get rid of fluid and relax vessels. Decongestants can cause fluid retention and vasoconstriction, undoing their benefits.
- Diuretics: Some decongestants contain hidden sodium. That makes diuretics less effective and can cause fluid buildup.
Worse, decongestants can interact dangerously with other common drugs like tricyclic antidepressants, linezolid (an antibiotic), and ergot-based migraine meds. These combinations can cause sudden, life-threatening spikes in blood pressure.
Who’s at the Highest Risk?
It’s not just people with very high blood pressure. Even those with well-managed hypertension are at risk. But some groups face greater danger:- People with uncontrolled hypertension (above 140/90)
- Those with heart disease, coronary artery disease, or a history of stroke
- People taking multiple blood pressure medications
- Older adults over 50-22% of emergency visits for uncontrolled high blood pressure in this group are linked to OTC decongestants
- Anyone with kidney disease, thyroid problems, or an enlarged prostate
Studies show only 38% of people with high blood pressure even know decongestants are risky. That’s why so many end up in trouble. It’s not ignorance-it’s misinformation. Many assume that because it’s sold over the counter, it’s safe. That’s a deadly assumption.
Safe Alternatives for Congestion Relief
You don’t need to suffer through a stuffy nose. There are safer ways to breathe:- Nasal saline spray - Plain saltwater spray or rinse (like a neti pot) is completely safe. It clears mucus without affecting your blood pressure.
- Humidifiers and steam - A hot shower or bowl of steam with a towel over your head loosens congestion naturally.
- Antihistamines - If your congestion is from allergies (not a cold), drugs like loratadine (Claritin) or cetirizine (Zyrtec) are generally safe for people on blood pressure meds. They don’t constrict blood vessels.
- Elevating your head - Sleeping with an extra pillow reduces nighttime congestion.
- Hydration - Drinking water thins mucus and helps your body clear it faster.
These alternatives might take a little longer to work, but they won’t put your heart at risk. And for mild colds, your body often clears things on its own in 5-7 days.
What to Do If You Must Use a Decongestant
Sometimes, your doctor might say it’s okay-rarely, and only for a few days. If that’s the case:- Use the lowest possible dose-never double up.
- Take it for no more than 3 days. Longer use increases risk.
- Monitor your blood pressure twice daily while taking it. If it jumps more than 15 points from your normal baseline, stop immediately.
- Never combine it with alcohol, caffeine, or stimulants-they add to the pressure spike.
- Always tell your pharmacist you’re on blood pressure meds. They’re trained to catch dangerous combinations.
Remember: if you’re unsure, skip it. Your pharmacist can help you pick a safe product-or better yet, suggest a non-decongestant option.
Reading Labels Like a Pro
You can’t trust the front of the box. Look at the Active Ingredients list on the back. Here’s what to watch for:- Pseudoephedrine
- Phenylephrine
- Oxymetazoline
- Ephedrine
- Any product labeled “Sinus,” “Congestion Relief,” or “All-in-One Cold & Flu”
Also watch for sodium content. Some cold medicines have over 200 mg of sodium per dose. The American Heart Association recommends under 1,500 mg per day for people with hypertension. One tablet could be 15% of your daily limit.
When to Call Your Doctor
Don’t wait for symptoms to get bad. Call your doctor if:- You’ve taken a decongestant and your blood pressure is higher than usual
- You feel your heart racing, pounding, or skipping beats
- You get chest tightness, dizziness, or blurred vision
- You’re unsure whether a product is safe
Your doctor might switch you to a different blood pressure med, adjust your dose, or recommend a safer cold remedy. They’ve seen this before. They want to help.

Pharmacists Are Your Secret Weapon
In the U.S., pseudoephedrine is kept behind the counter. That’s not just to stop drug makers-it’s to protect you. When you ask for it, the pharmacist is supposed to ask you questions: “Do you have high blood pressure?” “Are you on any heart meds?” “Have you had a heart attack?”Don’t brush them off. Use that moment. Say: “I’m on blood pressure medication. Is this safe?”
Studies show pharmacist-led reviews cut unsafe decongestant use by 47%. They know what’s in every bottle. They’re there to stop you from making a mistake.
Keep a Medication List
Write down everything you take-prescription, OTC, vitamins, herbal supplements. Include the dose and how often. Bring it to every doctor visit. Many people forget about the little things: cold meds, painkillers, sleep aids. But those are often the ones that cause trouble.When you show your list to your doctor or pharmacist, they can spot hidden risks. You might not realize that your nighttime cold remedy has a decongestant. They will.
What’s Changing in 2026?
This isn’t going away. The American College of Cardiology is updating its hypertension guidelines in early 2026 to include stronger warnings about OTC meds. Pharmaceutical companies are testing new decongestants that don’t constrict blood vessels-so far, in Phase 2 trials. But until those are available, the message stays the same: if you have high blood pressure, treat congestion the safe way.Can I use nasal sprays like Afrin if I have high blood pressure?
No. Even topical nasal sprays like Afrin (oxymetazoline) can be absorbed into your bloodstream and raise your blood pressure. They’re not safe for people on blood pressure medication unless your doctor says so-and even then, only for 2-3 days max. Long-term use can cause rebound congestion and worsen your condition.
Is phenylephrine safer than pseudoephedrine?
No. While pseudoephedrine is stronger, phenylephrine still raises blood pressure. A 2005 study found it causes a measurable increase in systolic pressure, especially at higher doses. Both are risky. Neither is safe for people with uncontrolled hypertension. If your cold medicine says it contains phenylephrine, treat it like a red flag.
Can I take antihistamines like Zyrtec with my blood pressure pills?
Yes, most antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are safe for people with high blood pressure. They work by blocking histamine, not by constricting blood vessels. But avoid antihistamines that also contain decongestants-check the label for pseudoephedrine or phenylephrine. Plain antihistamines are your best OTC option for allergy-related congestion.
How long does it take for blood pressure to return to normal after stopping a decongestant?
For most people, blood pressure starts dropping within 12-24 hours after stopping the decongestant. It usually returns to baseline within 2-3 days. But if your pressure stays high, your heart races, or you feel dizzy, seek medical help immediately. Some people, especially those with heart disease, may need monitoring or medication adjustment.
Are there any decongestants that are safe for high blood pressure?
There are currently no over-the-counter decongestants considered safe for people with high blood pressure without medical approval. Even the ones labeled “heart-safe” or “for sensitive users” still contain vasoconstrictors. The only safe options are saline sprays, humidifiers, antihistamines (without decongestants), and natural remedies. If you absolutely need a decongestant, your doctor may prescribe a short-term, low-dose option-but only after evaluating your specific health status.
Can decongestants cause long-term damage to blood pressure?
One or two short-term uses usually won’t cause permanent damage. But repeated use-especially without knowing it-can make your blood pressure harder to control over time. It can also mask the true effectiveness of your meds. If you’re regularly using decongestants, your doctor might think your hypertension is worsening when it’s actually the medication causing the spike. That can lead to unnecessary dose increases and more side effects.
Final Advice: When in Doubt, Skip It
Your nose might be stuffy, but your heart is more important. Every year, people think they’re being smart by treating a cold quickly. Instead, they end up in the hospital because they didn’t realize their medicine was working against them. You don’t need to suffer. You just need to be smart.Read every label. Talk to your pharmacist. Use saline sprays and steam. Ask your doctor before you take anything new-even if it’s sold on a shelf. Your blood pressure isn’t just a number. It’s your lifeline. Protect it like one.
Andy Heinlein
January 2, 2026 AT 11:54just took sudafed last week for my cold and felt like my heart was gonna explode lmao
glad i found this before i killed myself with a cold med
Layla Anna
January 3, 2026 AT 04:02my grandma uses saline spray and swears by it 😊
she says it's the only thing that doesn't make her dizzy
and she's been on bp meds for 20 years 💕
Matthew Hekmatniaz
January 3, 2026 AT 09:13really appreciate this breakdown. i used to think 'over-the-counter' meant 'safe for everyone'
turns out that’s like saying 'free sample' means 'no side effects'
pharmacists are the real MVPs here - never skip asking them
and yes, reading the back label is non-negotiable. i learned this the hard way after a 160/100 spike last winter
Austin Mac-Anabraba
January 4, 2026 AT 01:33the fact that pharmaceutical companies replaced pseudoephedrine with phenylephrine - a less effective but equally dangerous substitute - is not an accident. it’s corporate calculus.
they knew people would still buy it. they knew regulators wouldn’t push back. they knew you’d never read the fine print.
this isn’t negligence. it’s profit-driven predation disguised as consumer choice.
Phoebe McKenzie
January 5, 2026 AT 12:52how is this even legal??
you let people walk into a store and buy something that can KILL THEM and you call it 'over-the-counter'?
someone should sue every drug company and every pharmacy for manslaughter by negligence
my cousin died from this exact thing and no one even blinked
you people are lucky you're not in jail right now
gerard najera
January 6, 2026 AT 07:40decongestants = vasoconstriction.
vasoconstriction = increased afterload.
increased afterload = heart works harder.
heart works harder = bad.
simple.
Stephen Gikuma
January 7, 2026 AT 15:43they don't want you to know this - but the FDA and Big Pharma are in bed together.
they banned pseudoephedrine not because it's dangerous - but because it's used to make meth.
so they swapped it for phenylephrine - which does the same thing - so you keep buying it.
they don't care if you die - they care about the profit margin.
you're being played. wake up.
Bobby Collins
January 9, 2026 AT 13:35i think the government put oxymetazoline in sprays on purpose so people would get hooked and then need more meds to fix the rebound congestion
it's all a scheme
they want us dependent
and don't get me started on how they hide sodium in 'cold relief' pills
it's like a trap
you think you're helping your nose but you're slowly killing your kidneys
they know what they're doing
Ann Romine
January 9, 2026 AT 23:55my doctor actually gave me a list of safe OTC options after i asked - i never knew antihistamines like Zyrtec were okay
saline spray is my new best friend
also, i started keeping a medication list on my phone now - just a note with names and doses
it saved me last week when i almost grabbed a 'multi-symptom' cold pill
thank you for reminding me to read the back label
so many people don’t