Myasthenia gravis isn’t just muscle weakness-it’s weakness that gets worse the more you use your muscles. You might lift your arm once, then struggle to do it again five minutes later. Eyelids droop after reading for a few minutes. Swallowing becomes a chore. Speaking turns into a slurred mess. And then, after resting, everything comes back-almost normal. That’s the hallmark of myasthenia gravis: fatigable weakness. It doesn’t follow the rules of ordinary tiredness. It’s neurological, autoimmune, and deeply unpredictable.
What Causes Myasthenia Gravis?
At the core of myasthenia gravis is a breakdown in communication between nerves and muscles. Normally, a nerve releases acetylcholine, a chemical messenger that tells a muscle to contract. In myasthenia gravis, the body’s own immune system attacks the receptors on the muscle that receive this signal. Antibodies latch onto the acetylcholine receptors (AChR), blocking or destroying them. Without enough receptors, the muscle can’t respond properly-no matter how strong the nerve signal is. About 80-90% of people with generalized myasthenia gravis have these AChR antibodies. Another 5-8% have antibodies against a different protein called MuSK. The rest are seronegative-no known antibodies are detected, but the disease still behaves the same way. This isn’t random. The immune system is literally turning against itself. The condition was first described in the 1600s, but it wasn’t until 1973 that scientists proved these antibodies were the cause by injecting them into animals and reproducing the disease.Who Gets Myasthenia Gravis?
It can strike at any age, but there are two clear patterns. People under 50-especially women-are more likely to develop early-onset myasthenia gravis. Their thymus gland, an organ involved in immune training, is often enlarged or abnormal. In fact, up to 75% of these patients have thymic hyperplasia. For those over 50, the risk shifts. Thymomas-tumors of the thymus-appear in 10-15% of late-onset cases. These tumors aren’t always cancerous, but they’re linked to more aggressive disease. About 15-20% of people start with only eye symptoms: drooping eyelids or double vision. That’s called ocular myasthenia. But here’s the catch-half to 80% of them will develop full-body weakness within two years. That’s why even mild eye symptoms need monitoring. It’s not just about vision-it’s a warning sign the immune system is expanding its attack.Fatigable Weakness: The Signature Symptom
The term "fatigable weakness" is what sets myasthenia gravis apart from other muscle diseases. It’s not about being worn out after a workout. It’s about muscles failing mid-task. Try holding your arm up for 30 seconds. Now try again after a short break. If it’s much harder the second time, that’s fatigable weakness. It’s the same with chewing-food gets harder to swallow as you eat. Speaking becomes slurred after a few sentences. Climbing stairs feels impossible after the third step. Doctors use a tool called the Quantitative Myasthenia Gravis Score (QMGS) to measure severity. A score above 11 means the disease is moderate to severe and needs more than just symptom relief. That’s when immunotherapy becomes necessary. The weakness doesn’t follow a pattern of constant decline. It flares, fades, and returns. One day you feel fine. The next, you can’t lift a coffee cup. That unpredictability is what makes it so hard to live with.First-Line Treatments: Symptom Control and Immune Suppression
Treatment has two goals: ease symptoms right away, and calm the immune system long-term. The first drug most people get is pyridostigmine. It works by slowing down the breakdown of acetylcholine, giving the remaining receptors more time to do their job. Doses range from 60 to 240 mg a day, split into multiple doses. It helps-but it doesn’t stop the immune attack. That’s where immunotherapy comes in. Corticosteroids like prednisone are the most common immunosuppressant. About 70-80% of patients see major improvement or even complete symptom relief on steroids. But there’s a cost. Weight gain, mood swings, bone thinning, diabetes-side effects hit hard. About 70% of people on long-term prednisone (over 10 mg daily) gain weight. That’s why doctors try to get patients off steroids as soon as possible. That’s where steroid-sparing drugs come in. Azathioprine and mycophenolate mofetil are the go-to options. Azathioprine takes 6-18 months to work, but once it does, about 60-70% of patients can reduce or stop steroids. Mycophenolate works a bit faster, with 50-60% effectiveness. Both need regular blood tests because they can damage the liver or lower white blood cell counts. About 15-20% of people on azathioprine have to stop because of side effects.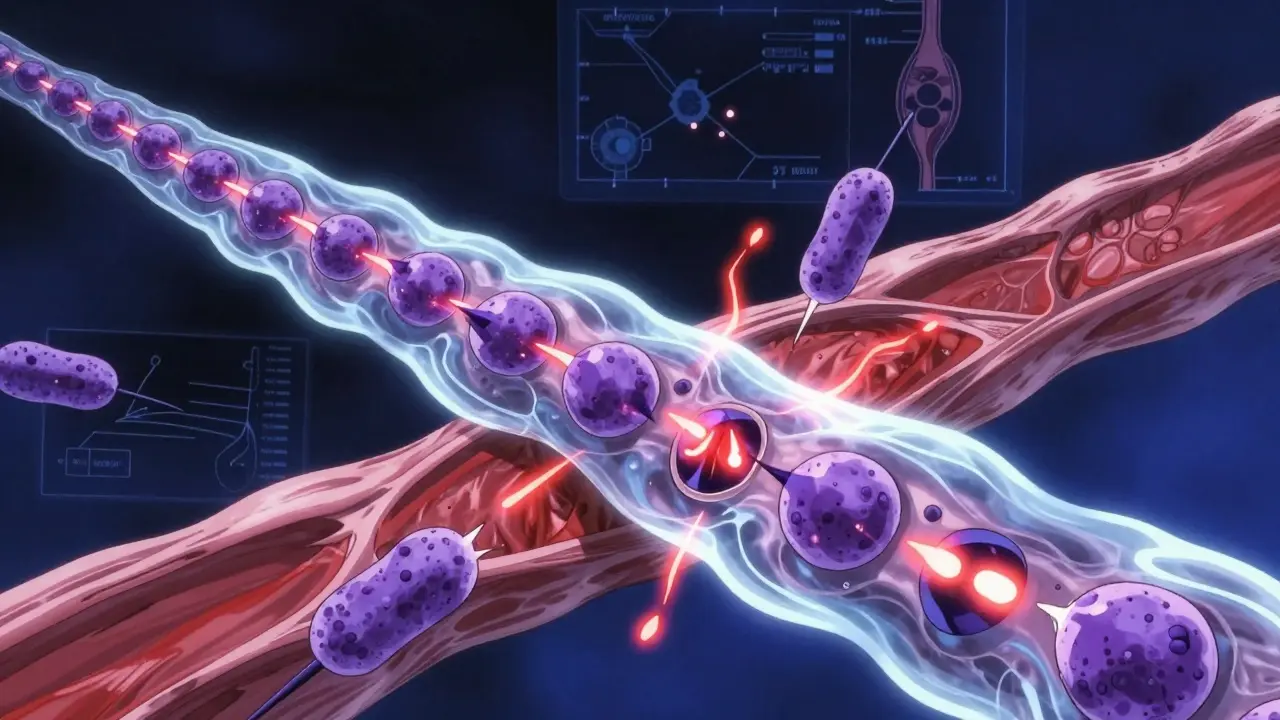
Fast-Acting Options for Crises
Sometimes, myasthenia gravis flares into a medical emergency. Breathing muscles weaken. Swallowing becomes dangerous. That’s a myasthenic crisis. When that happens, you need fast results-not months of waiting. Two treatments work quickly: intravenous immunoglobulin (IVIG) and plasma exchange (PLEX). Both remove or block the bad antibodies. IVIG gives you antibodies from healthy donors that confuse the immune system. It takes 5-7 days to work, but it’s well tolerated. PLEX literally filters your blood to pull out the harmful antibodies. It works faster-2-3 days-and is often preferred if breathing is in danger. But it requires a central line, carries infection risks, and isn’t something you can do at home. Both give relief for 3-6 weeks. They’re not cures. They’re emergency brakes. But they buy time while slower treatments kick in.Thymectomy: Removing the Source
For people with early-onset, AChR-positive myasthenia gravis, removing the thymus gland (thymectomy) isn’t optional-it’s recommended. The MGTX trial showed that patients who had surgery along with medication reached stable remission three times faster than those on medication alone. After five years, 35-45% of those who had thymectomies were in complete remission-no drugs needed. The surgery is usually done through minimally invasive techniques now. Recovery takes weeks, not months. For patients aged 18-65 with generalized disease, it’s standard care. Even if you don’t feel better right away, the long-term benefit is real. It changes the course of the disease.Next-Generation Immunotherapies
The biggest breakthroughs in the last five years aren’t just tweaks-they’re entirely new ways to fight the disease. The FDA approved efgartigimod in 2021. It’s not a steroid. It’s not a chemotherapy drug. It’s a targeted blocker of the neonatal Fc receptor (nFcR), a molecule that recycles antibodies in the body. By blocking it, efgartigimod causes a 60-75% drop in all IgG antibodies-including the bad ones-in just a week. In clinical trials, 68% of patients reached minimal manifestation status. No more daily steroids. No more monthly infusions. Just a weekly shot under the skin. Ravulizumab, approved in 2023, blocks a different part of the immune response-the complement system. It’s the first complement inhibitor for myasthenia gravis. It’s given every 8 weeks, and early data shows it helps patients stay stable with fewer relapses. These drugs are changing lives. But they’re expensive. And we don’t yet know the long-term safety beyond two years. Still, for people who’ve tried everything else, they’re a lifeline.
What Doesn’t Work-and What Can Make Things Worse
Not every treatment helps every type of myasthenia gravis. Rituximab, a drug that wipes out B-cells, works wonders for MuSK-positive patients-71-89% improve. But in AChR-positive cases, it’s only about 40-50% effective. That’s why testing for antibodies isn’t just paperwork-it’s the key to picking the right drug. And then there’s the dark side: immune checkpoint inhibitors. These cancer drugs-used for melanoma, lung cancer, and others-can trigger myasthenia gravis in people who never had it before. In 60% of these cases, the disease comes with heart inflammation (myocarditis). About 83% of these patients end up in the ICU. If you have myasthenia gravis and are considering cancer immunotherapy, talk to a neurologist first. The risk isn’t theoretical-it’s life-threatening.Living With Myasthenia Gravis
Most people with myasthenia gravis need long-term treatment. About 85-90% stay on some form of immunosuppression. But that doesn’t mean a poor quality of life. With the right mix of drugs, lifestyle adjustments, and regular monitoring, most patients reach a point where symptoms are barely noticeable. That’s called minimal manifestation status. The key is patience. Drugs like azathioprine take over a year to work. Steroids can’t be stopped too fast-tapering too soon leads to relapse in 40-50% of cases. And thymectomy? It’s not a quick fix. The benefits show up over years, not weeks. Avoiding infections is critical. Being on immunosuppressants means your body can’t fight off bugs as well. Flu shots, pneumonia shots, and avoiding sick people aren’t optional. Many patients keep a supply of IVIG or steroids at home for sudden flares.What’s Next?
The future of myasthenia gravis treatment is focused on stopping the disease, not just managing it. Over 15 clinical trials are testing new drugs that target specific immune cells, cytokines, or pathways. The goal? To get people off drugs entirely. To achieve remission without lifelong immunosuppression. Some of the most promising candidates include rozanolixizumab and inebilizumab-both designed to be given at home, with fewer side effects than current options. The Myasthenia Gravis Foundation’s 2023 research roadmap calls this the top priority: disease modification without chronic treatment. We’re no longer just treating symptoms. We’re reprogramming the immune system.Is myasthenia gravis curable?
There’s no universal cure, but many people achieve long-term remission-especially those with early-onset, AChR-positive disease who have a thymectomy. Around 35-45% of these patients stop needing medication after five years. Others manage the disease so well that symptoms are barely noticeable. Complete remission without drugs is possible, but rare. Most people need ongoing treatment, but modern therapies let them live full, active lives.
Can stress make myasthenia gravis worse?
Yes. Stress, whether emotional or physical, can trigger flares. Illness, surgery, lack of sleep, and even intense exercise can worsen weakness. That’s why managing stress and avoiding overexertion are part of treatment. It’s not about avoiding all activity-it’s about pacing. Rest before you hit the wall. Plan your day around energy peaks. Many patients find that short walks, yoga, or swimming help maintain strength without triggering fatigue.
Why do some people with myasthenia gravis need a ventilator?
When the muscles that control breathing weaken too much, it leads to a myasthenic crisis. This is a medical emergency. The diaphragm and other breathing muscles can’t keep up, leading to low oxygen levels. About 15-20% of patients will experience this at some point. It’s why having a plan with your neurologist is critical-knowing when to go to the hospital, having emergency IVIG or PLEX on standby, and recognizing early signs like rapid breathing, muffled speech, or trouble swallowing saliva can save your life.
Are there foods or diets that help with myasthenia gravis?
No specific diet cures or reverses myasthenia gravis. But swallowing difficulties mean some foods are harder to manage. Soft, moist foods are easier than dry or crumbly ones. Eating smaller meals more often helps avoid fatigue while chewing. Avoiding alcohol and certain antibiotics (like fluoroquinolones or macrolides) is important-they can worsen muscle weakness. Some patients benefit from nutritional supplements if weight loss becomes an issue. Always talk to your doctor before making big dietary changes.
Can I still exercise with myasthenia gravis?
Yes-but carefully. Regular, gentle exercise helps maintain muscle strength and prevents deconditioning. Walking, swimming, and light resistance training are often recommended. The key is to stop before you feel exhausted. Pushing through fatigue can make symptoms worse for hours or days. Many patients use pacing techniques: 10 minutes of activity, 20 minutes of rest. Working with a physical therapist who understands neuromuscular diseases is the best way to build a safe routine.
How often do I need blood tests on immunosuppressants?
It depends on the drug. For azathioprine, blood counts and liver function are checked every 2-4 weeks at first, then every 3 months once stable. Mycophenolate requires similar monitoring. Steroids need occasional glucose and bone density checks. These tests aren’t just routine-they catch problems early. Liver damage or low white blood cells can be silent until it’s too late. Regular monitoring is non-negotiable for long-term safety.
