Why Medication Management at Home Matters for Seniors
Managing medications at home isn’t just about popping pills on time. For seniors taking five or more drugs daily, one missed dose or wrong combination can lead to a hospital trip-or worse. Around 30% of all adverse events in home care come from medication mistakes, according to MedPro’s 2022 risk analysis. That’s not a small number. It’s the difference between staying safe at home and ending up back in the ER.
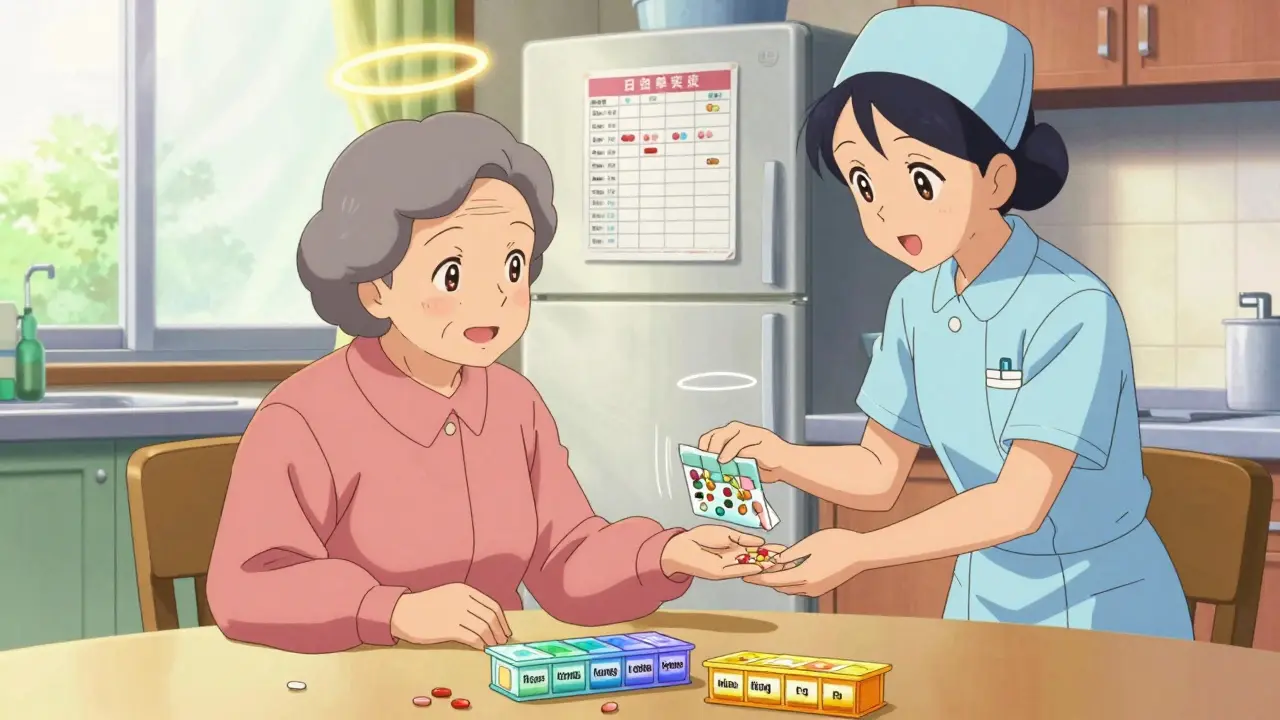
Home health services step in to fix this. These aren’t just visiting nurses dropping by. They’re trained professionals who track every pill, check for dangerous interactions, and make sure the right dose goes in at the right time. The result? A 20% drop in 30-day hospital readmissions, as shown by Clarest’s 2023 data. That’s real savings-for families, for the system, and most importantly, for the person taking the meds.
What Exactly Do Home Health Services Do for Medication Management?
It’s more than handing out pills. A good home health agency does four big things:
- Updates the medication list-every drug, even over-the-counter ones like ibuprofen or vitamin D. They write down brand names, generics, dosages, why it’s prescribed, and any known side effects. This list gets shared with every doctor involved.
- Uses tools to prevent errors-think pill organizers with compartments for morning, afternoon, evening, and bedtime. Some agencies, like Phoenix Home Care, use pre-filled daily pouches labeled with the exact time and drug name. These cut missed doses by up to 45%, according to the Caregiver Action Network.
- Tracks timing and adherence-they set alarms on phones or use digital apps that send reminders. One study found these reminders improve adherence by 35%. For someone with dementia or poor eyesight, that’s life-changing.
- Does medication reconciliation-every time a patient leaves the hospital or switches doctors, the home health team checks: Are any drugs duplicated? Are any no longer needed? Are new ones safe with the old ones?
This isn’t optional. CMS requires it. If a home health agency doesn’t do this right, they risk losing Medicare reimbursement.
How to Get Home Health Services for Medication Management
Not everyone qualifies, but many more people think they don’t than actually don’t.
If you’re on Medicare Part A, you can get home health services at no extra cost-if you meet three criteria:
- You’re homebound (leaving home takes a lot of effort or medical risk)
- You need skilled nursing or therapy (like wound care, injections, or medication training)
- A doctor certifies you need these services
Medicare doesn’t cover daily help with pills if that’s all you need. But if you’re recovering from surgery, had a stroke, or were just discharged from the hospital with a complex new drug plan? You’re likely covered.
If you don’t qualify for Medicare-covered services, private agencies like Clarest charge $20-$40 per hour for medication management. Some long-term care insurance policies cover this. Check your policy. Don’t assume it doesn’t.
What to Look for in a Home Health Agency
Not all agencies are the same. Here’s what to ask before signing up:
- Do they use a standardized medication reconciliation process? Ask if they check for duplicates, interactions, and outdated prescriptions every time care changes.
- Do they use visual aids? Look for agencies that print medication charts in large font, with pictures or color codes. One survey found 67% of caregivers said this made a huge difference.
- Do they offer multilingual support? If English isn’t the patient’s first language, ask if instructions come in their native tongue. Phoenix Home Care added QR codes linking to video instructions in 17 languages in 2023.
- How do they handle emergencies? Ask for a printed list of all meds and provider contacts. It should be taped to the fridge or kept in a wallet.
- What’s their staff turnover rate? High turnover means inconsistent care. Ask how long nurses typically stay with one patient.
Also, check if the agency is Medicare-certified. That means they follow federal rules. You can verify this on Medicare.gov’s Home Health Compare tool.
What Doesn’t Work-and Why
Some families try to manage meds themselves. They use a pillbox from the pharmacy. They set phone alarms. They think, “I’ve got this.”
But here’s what often goes wrong:
- Duplicate prescriptions-two doctors each prescribe the same drug, and no one checks. One case study found 12 dangerous duplicates avoided in just six months by one agency’s staff.
- Wrong timing-some meds need to be taken on an empty stomach. Others must be spaced 12 hours apart. If you’re not trained, you’ll miss this.
- Ignoring side effects-dizziness, confusion, nausea. Seniors often think it’s just “getting older.” But it could be a drug reaction.
- Not updating the list-if a doctor stops a drug, but the list isn’t changed, the nurse keeps giving it. That’s how errors happen.
And here’s the big one: communication gaps. One Reddit user shared how inconsistent info between providers led to a dangerous blood thinner interaction. That’s not rare. Only 65% of agencies do full reconciliation during care transitions, even though CMS says they must.
Real Stories: What Works
Mary K. from Ohio had her 82-year-old mother on seven medications. She was missing doses 30% of the time. “I was exhausted,” she said. “I’d come home from work and find half the pills still in the box.”
After hiring Phoenix Home Care and switching to their WellPack daily pouches, missed doses dropped to under 5% in two weeks. “It wasn’t magic,” Mary said. “It was just clear labels and someone checking in every day.”
John T., who cared for his father with Parkinson’s, tried managing meds alone. He didn’t know his dad’s new blood pressure med interacted with his heart drug. He ended up in the ER. “I thought I was helping,” he said. “I didn’t know what to look for.”
After getting home health support, John got a printed med list, a digital reminder app, and a nurse who called every Monday to review changes. “Now I sleep better,” he said.
Technology Is Helping-But Not Replacing People
Apps with alarms, biometric verification, and QR code videos are growing fast. CritiCare’s app, launched in March 2023, cut administration errors by 40% in its pilot group. Some agencies are testing AI that flags dangerous drug combos before they’re prescribed.
But tech alone won’t fix everything. Seniors with memory loss, vision problems, or hearing loss still need a person to confirm the pill went in, to notice if they’re slurring words after a new med, or to call the doctor if they’re unusually tired.
The best systems combine tech and touch. A digital reminder wakes them up. A nurse shows up, watches them swallow the pill, and writes it down. That’s the gold standard.

What to Do If You Can’t Get Home Health Services
If you don’t qualify for Medicare-covered care or can’t afford private help, here’s what you can still do:
- Make a simple med list-write down every drug, dose, time, and why. Use big print. Keep two copies: one at home, one with a family member.
- Use a pill organizer-buy one with AM/PM/Evening/Bedtime compartments. Don’t rely on memory.
- Set phone alarms-label them: “Take Lisinopril,” “Take Metformin,” etc. Use multiple alarms if needed.
- Ask for a med review-every 6 months, ask the primary care doctor to go over all meds. Use the Beers Criteria to ask: “Are any of these unsafe for someone my age?”
- Get a backup-train a neighbor, church volunteer, or local senior center aide to check in once a week to make sure pills are being taken.
It’s not perfect. But it’s safer than doing nothing.
How Often Should Medication Management Be Reviewed?
Not once a year. Not when you feel bad. Every time something changes.
- After a hospital stay
- When a new doctor prescribes something
- When a drug is stopped
- Every 3 months if taking 5+ meds
- Every 6 months even if things seem stable
MedPro’s data shows that regular reviews reduce adverse events by 60% compared to self-management. That’s the biggest safety net you can have.
Final Thoughts: It’s Not About Control. It’s About Safety.
Many seniors want to manage their own meds. They fear losing independence. But true independence isn’t doing it alone. It’s being safe, healthy, and in control of your life.
Home health services for medication management aren’t a sign of failure. They’re a smart, proven way to avoid hospital stays, prevent dangerous mistakes, and keep people living well at home.
Ask for help. Don’t wait for a crisis. Start the conversation with your doctor today. Your body, your peace of mind, and your family will thank you.
Can Medicare cover home health services for medication management?
Yes, but only under specific conditions. Medicare Part A covers home health services if you’re homebound, need skilled nursing care (like medication training or injections), and have a doctor’s order. It doesn’t cover daily pill reminders alone. But if you’re recovering from surgery or have complex meds after a hospital stay, you likely qualify. No extra cost if you meet the criteria.
What’s the difference between a pill organizer and a home health service?
A pill organizer is a tool-it holds pills in time slots. A home health service is a person-a trained nurse or aide who checks your meds, updates your list, watches for side effects, calls your doctor if something’s wrong, and confirms you actually take the pill. The organizer helps with memory. The service prevents errors and saves lives.
Can home health services handle psychiatric medications?
They can manage them, but not always adjust them. Home health staff can give antipsychotics or antidepressants as prescribed. But if doses need frequent changes based on mood or behavior, they’ll need direction from a psychiatrist. Complex psychiatric regimens often require more frequent oversight than most home health agencies can provide without extra support.
How do I know if a medication is unsafe for an older adult?
Ask your doctor to use the Beers Criteria-a list of medications that are often risky for seniors, like certain sleep aids, antihistamines, or painkillers. Common red flags: dizziness, confusion, falls, or constipation after starting a new drug. Don’t assume it’s just aging. Bring your full med list to every appointment.
What should I do if I notice a medication error?
Stop giving the medication immediately. Call the prescribing doctor or pharmacist. If the person seems unwell-confused, fainting, having trouble breathing-call 999. Then, report the error to the home health agency. They’re required to document and investigate it. Keep a written record of what happened, when, and who you talked to.
Are digital medication apps reliable?
They’re helpful, but not foolproof. Apps with alarms and reminders improve adherence by 35%, but they can’t confirm if the pill was swallowed. They also don’t catch drug interactions or side effects. Use them as a backup, not the only system. The best approach combines digital reminders with a human check-in.
How much does private home health medication management cost?
Private agencies typically charge $20-$40 per hour in the UK and US. Some offer daily visits for complex regimens, which can cost $100-$200 per week. Check if your long-term care insurance covers it. Some Medicaid waivers or VA benefits may also help. Always ask for a written service agreement before starting.
Next Steps: What to Do Today
Don’t wait for a problem to happen.
- Today: Write down every medication your loved one takes-prescription, over-the-counter, vitamins, supplements. Include the dose and why.
- This week: Call their primary care doctor and ask: “Can we do a full medication review using the Beers Criteria?”
- This month: Contact your local Medicare-certified home health agency. Ask if they offer medication management and what the eligibility rules are.
- Always: Keep a printed copy of the med list on the fridge and in a wallet. Make sure someone else has a copy too.
Medication safety isn’t a one-time task. It’s a daily habit. And with the right support, it’s one that can be managed-with dignity, safety, and peace of mind.
Caitlin Foster
December 26, 2025 AT 15:45James Bowers
December 28, 2025 AT 12:07Will Neitzer
December 30, 2025 AT 10:35Janice Holmes
December 31, 2025 AT 17:19Olivia Goolsby
January 1, 2026 AT 08:04Alex Lopez
January 2, 2026 AT 21:41Monika Naumann
January 3, 2026 AT 11:15Elizabeth Ganak
January 4, 2026 AT 12:51Nicola George
January 6, 2026 AT 07:23