Switching from a brand-name medication to a generic version sounds simple: same active ingredient, lower cost, right? But for some people, that switch isn’t just about money-it’s about how their body reacts. If you’ve noticed changes in how you feel after your pharmacy filled a generic version of your prescription, you’re not alone. And you have every right to talk to your doctor about staying on the brand.
Why Some People Need to Stay on Brand Medication
Not all generics are created equal in how they affect your body. The FDA says generics must be bioequivalent to brand-name drugs, meaning they deliver the same active ingredient at the same rate and amount. But here’s the catch: bioequivalence doesn’t mean identical. Generics can differ in inactive ingredients-like dyes, fillers, preservatives, or coatings. These might seem harmless, but for some people, they trigger real problems.For example, if you’re on levothyroxine for thyroid issues, even tiny changes in absorption can throw your hormone levels off. A 2021 study in Neurology found that switching from brand-name anti-seizure drugs to generics led to a 23% higher chance of seizure recurrence. Patients on warfarin, a blood thinner, saw a 17% spike in emergency visits after switching between generic manufacturers. Why? Because these drugs have a narrow therapeutic index-small changes in blood levels can mean big health risks.
And it’s not just about effectiveness. About 7% of patients report allergic reactions or intolerances to inactive ingredients in generics. Lactose, gluten, or artificial colors can cause bloating, rashes, or headaches in sensitive individuals. If you’ve ever felt off after a pill change but couldn’t explain why, it might be one of these hidden ingredients.
What to Say to Your Doctor
Talking to your doctor about staying on brand doesn’t mean arguing. It means showing up prepared. Start by documenting what happened. Keep a simple log: when you switched, what symptoms appeared, and when they improved after going back to the brand. Include dates, severity (on a scale of 1-10), and any lab results that changed-like INR levels for warfarin or TSH for thyroid meds.Use clear, specific language. Instead of saying, “I don’t trust generics,” say: “After switching to the generic version of my seizure medication, I had three seizures in two months. I hadn’t had one in five years on the brand. When I went back to the original, they stopped.” That’s data. That’s hard to ignore.
Bring your medication bottles to the appointment. Point out the inactive ingredients listed on the generic label and compare them to the brand. If you know your body reacts to certain dyes or fillers, say so. Your doctor needs to understand this isn’t preference-it’s medical necessity.
Use the SBAR method: Situation, Background, Assessment, Recommendation. For example:
- Situation: “I had a seizure last week.”
- Background: “I switched to generic Keppra three months ago. Before that, I was on the brand for five years with no seizures.”
- Assessment: “My neurologist’s notes from last year show stable levels on the brand. My recent blood test shows a drop in drug concentration.”
- Recommendation: “I’d like to stay on the brand unless there’s a safer, proven alternative.”
This approach works. A 2022 study in the AMA Journal of Ethics found that using SBAR increased successful outcomes in 78% of cases where patients requested brand-name drugs.
Insurance and Prior Authorization
Most insurance plans push for generics because they’re cheaper. But that doesn’t mean you’re stuck. Your doctor can request a prior authorization for the brand-name drug. This means they’ll submit documentation to your insurer explaining why the generic won’t work for you.What does that look like? They’ll need:
- Proof of therapeutic failure with the generic (lab results, symptom logs)
- Documentation of allergic reaction to inactive ingredients
- Evidence that switching caused a decline in your condition
According to a 2023 Kaiser Family Foundation report, 72% of insurance denials for brand-name drugs are overturned when you appeal with solid documentation. That’s more than two out of three. Don’t give up after the first “no.”
Ask your doctor to write “Dispense as Written” (DAW-1) on the prescription. This code tells the pharmacy: “Do not substitute.” Some states require patient consent before substitution, but 47 states let pharmacists swap generics without asking. DAW-1 gives you legal backing.
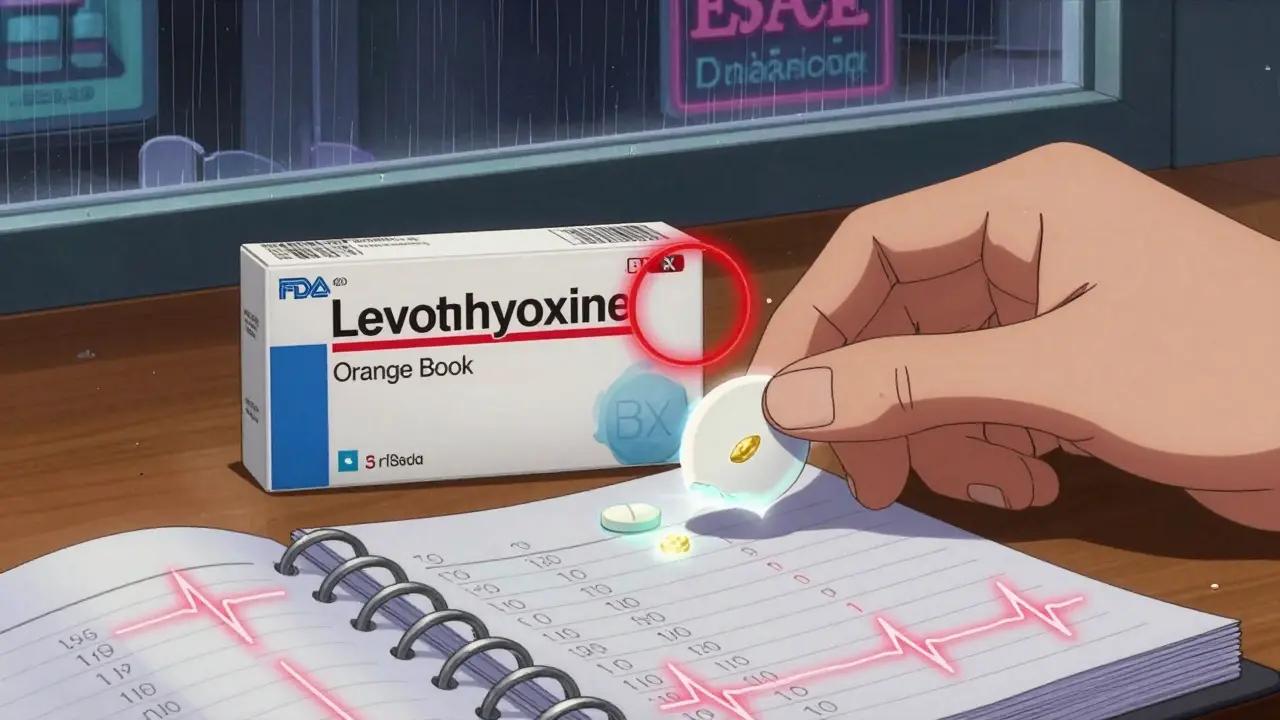
How to Get the Evidence You Need
You don’t need to guess what’s in your meds. Use the FDA’s Orange Book (available online). Search for your drug by name. It lists all approved brand and generic versions, their active ingredients, and whether they’re rated as therapeutically equivalent. If your brand has an “AB” rating, it’s considered interchangeable. But if it’s “BX,” that means there’s no generic that’s proven equivalent-your doctor can use that to argue for staying on brand.Also, check the inactive ingredients. The FDA’s Drugs@FDA database lets you look up the exact formulation of your brand-name drug. Print the list and bring it to your appointment. If your generic has a dye you know you’re sensitive to, highlight it. This isn’t paranoia-it’s precision.
Pharmacists can help too. Ask them to compare the inactive ingredients between your brand and the generic. Many will gladly do it. They see these switches every day. Some even tell patients: “I’ve seen people react to the gluten in this generic version. I’d stick with the brand if I were you.”
What About Cost?
Yes, brand-name drugs cost more. But ask yourself: what’s the real cost of a bad reaction? Emergency room visits, missed work, hospital stays-they add up fast. A 2022 study in the American Journal of Managed Care found that patients who switched generic warfarin had 17% more ER visits. That’s not just money-it’s risk.Some drug manufacturers offer patient assistance programs. If you’re on a brand like Keppra, Lamictal, or Synthroid, check the company’s website. Many have co-pay cards or free trials. Medicare Part D has an exceptions process too-57% of requests for brand-name drugs are approved when you submit proper clinical records.
If your insurance still refuses, ask your doctor about an appeal. Submit your symptom log, lab results, and pharmacy records. You’re not asking for special treatment. You’re asking for safe, effective care.

When Generics Are Fine-and When They’re Not
Most people switch to generics without issue. For antibiotics, blood pressure meds, or antidepressants, generics work just as well. But for drugs where tiny changes matter, the risks are real:- Thyroid meds (levothyroxine) - Small absorption differences affect hormone balance
- Anti-seizure drugs (Keppra, Lamictal) - Higher seizure risk after switching
- Blood thinners (warfarin) - Unstable INR levels lead to bleeding or clots
- Immunosuppressants (cyclosporine, tacrolimus) - Risk of organ rejection
- Psychiatric drugs (lithium, valproate) - Mood swings, relapse
If you’re on one of these, don’t assume the generic is safe. Ask your doctor: “Is this one of those drugs where switching could be risky?”
What to Do Next
Start today. Don’t wait until you’re in crisis.- Check your current prescription-is it a brand or generic?
- Look up your drug on the FDA’s Orange Book. Note its therapeutic rating.
- Review your symptom history. Did anything change after a switch?
- Write down your concerns. Bring them to your next appointment.
- Ask your pharmacist to compare the inactive ingredients.
- Request a DAW-1 code on your prescription.
You know your body better than anyone. If something feels off after a medication change, trust that feeling. You’re not being difficult-you’re being responsible. And you have the right to ask for what keeps you healthy.
Can my pharmacist substitute a generic without my permission?
In 47 U.S. states, pharmacists can switch your brand-name drug to a generic without telling you or getting your doctor’s approval. Only 12 states require patient consent. To prevent this, ask your doctor to write "Dispense as Written" (DAW-1) on your prescription. This legally blocks substitution.
Are generics less effective than brand-name drugs?
For most medications, yes-they’re equally effective. But for drugs with a narrow therapeutic index-like thyroid meds, seizure drugs, or blood thinners-even small differences in how the body absorbs the drug can lead to serious side effects or treatment failure. Studies show higher rates of seizures, hospital visits, and unstable lab values after switching these specific drugs to generics.
How do I prove I need to stay on brand?
Keep a symptom journal with dates and severity. Save lab results that show changes after switching (like INR, TSH, or drug levels). Bring your old and new pill bottles to your appointment. Ask your doctor to document your history of adverse reactions. This evidence is what insurers and doctors need to approve a brand-name exception.
What if my insurance denies my request?
Appeal the decision. Submit your symptom log, lab results, and doctor’s note. About 72% of denials are overturned on appeal when you provide clear clinical evidence. Your doctor can help file the appeal. Some manufacturers also offer patient assistance programs to reduce out-of-pocket costs.
Is it worth the extra cost to stay on brand?
If you’ve had a bad reaction to a generic, yes. Emergency room visits, hospitalizations, or missed work due to medication failure cost far more than the price difference. For drugs like warfarin or levothyroxine, staying on brand can prevent life-threatening complications. Talk to your doctor about cost-saving options-many brands offer coupons or patient support programs.