Why Medication Adherence Crashes During Life Changes
Imagine this: you’ve been taking your blood pressure pills every morning like clockwork for two years. Then you get laid off, move to a new city, and your partner moves out-all within three weeks. Suddenly, you’re sleeping on a friend’s couch, working temp jobs, and your pills are still in a box you haven’t unpacked. This isn’t laziness. It’s non-adherence during stress, and it happens to more than half of people going through major life shifts.
Research from the Journal of Personality and Social Psychology shows medication adherence drops by an average of 32% during high-stress transitions. The American Psychological Association found that 68% of chronic disease setbacks happen in the first three months after a big change-divorce, job loss, moving, or even starting a new job. It’s not that people stop caring. It’s that their routines, their reminders, their sense of control-all of it-gets ripped away.
And the cost? Real. A 2022 study in the New England Journal of Medicine found that fixing adherence during transitions could cut hospital readmissions by up to 24%. In the U.S. alone, preventable non-adherence costs the system $100-300 billion a year. This isn’t a personal failure. It’s a system gap.
What You Can Actually Control (And What You Can’t)
When your world is falling apart, the last thing you need is to feel guilty for forgetting your pills. But here’s the secret: your brain doesn’t care about guilt. It cares about control. And when you feel powerless, your body shuts down non-essential tasks-like taking medicine.
Psychological research from the Psychological Bulletin (2021) shows that people who focus on what they can control improve adherence by nearly 20%. So here’s how to do it:
- Things you can control directly (27.3%): Where you keep your pills. When you take them. Who you tell about your routine. Whether you refill your prescription on time.
- Things you can influence (43.8%): Your sleep schedule, your stress levels, whether you ask your doctor for help, if you use a reminder app.
- Things outside your control (28.9%): Your boss’s schedule, your ex’s new partner, the weather, the pharmacy’s closing time.
Stop wasting energy on the third list. That’s where most people get stuck-worrying about things they can’t change. Redirect that energy to the first two. If you can’t control your move, you can still control where you put your pillbox. If you can’t control your anxiety, you can still control when you take your meds-right after brushing your teeth, or right before your morning coffee.
Build Flexible Routines, Not Rigid Schedules
When your life is stable, a 7 a.m. pill works fine. But when you’re moving apartments, starting a new job, or recovering from a breakup, rigid schedules collapse. That’s why sticking to the same time every day often fails during transitions.
Instead, anchor your medication to habits that don’t change. Research from the Journal of Personality and Social Psychology shows that keeping just 3-5 daily anchor activities reduces stress by 23% and improves adherence by over 31%. These anchors are things you do no matter what:
- Washing your face
- Drinking your first sip of water
- Checking your phone in the morning
- Turning off the lights at night
Attach your pill to one of these. Not “take it at 8 a.m.” but “take it after I wash my face.” That way, even if you’re sleeping on a floor in a new city, you still do your face. And then you take your pill. No calendar needed.
Time-blocking works better than strict scheduling during transitions. Don’t say “I’ll take my meds at 8 a.m.” Say “I’ll take my meds in the morning, before I leave the house.” That gives you 2-3 hours of flexibility. You’re less likely to miss it.
Why Reminder Apps Fail During Stress (And What Works Better)
You’ve probably tried a pill reminder app. Maybe it worked fine-until your life changed. A 2023 study in the Journal of Medical Internet Research found that while apps improve adherence by 22.8% during normal times, that benefit drops to just 8.3% during big transitions. Why? Because apps assume you’re still in control. They don’t adapt when your routine shatters.
But some apps do. Tools like TransitionAdhere and LifeShiftRx have 4.2-star ratings because they’re built for chaos. They don’t just remind you. They ask: “Are you moving? Starting a new job? Going through a breakup?” Then they adjust. They offer pre-made plans for 12 common transitions. You pick yours, and the app reorganizes your reminders, connects you to local pharmacies, and even texts you a checklist: “Pack your meds. Call your new doctor. Save the pharmacy number.”
For most people, though, you don’t need a fancy app. You need a simple list. Write down: “What I need to do before I leave this place” and “What I need to do after I arrive.” Include: refill prescriptions, get new insurance info, find a pharmacy, tell someone your routine. Do this before the transition hits. Don’t wait until you’re overwhelmed.
Therapy Isn’t Just for Mental Health-It’s for Medication Adherence
Most people think therapy is for anxiety or depression. But if you’re struggling to take your meds during a transition, therapy might be the most practical thing you can do.
Acceptance and Commitment Therapy (ACT) isn’t about fixing your emotions. It’s about learning to act even when things are hard. A 2022 JAMA Internal Medicine trial found ACT improved medication adherence by 48.6% during life changes-far more than standard counseling or reminders.
Here’s how it works in practice:
- You don’t say, “I have to take my pills.” You say, “Taking my pills is how I show up for myself-even when I’m scared.”
- You don’t fight the urge to skip. You notice it: “I’m feeling overwhelmed. My body wants to stop.” Then you take the pill anyway.
- You connect your medicine to your values: “I take this because I want to be here for my kid. Because I want to walk without pain. Because I’m not done living.”
You don’t need a therapist to start. Try this: Write down one reason your medication matters to you. Tape it to your mirror. Read it every morning. That’s ACT in five minutes.
Ask for Help-Before You Need It
One of the biggest mistakes people make? Waiting until they’ve missed doses to say something. By then, the damage is done.
Dr. Linda Rodriguez of the National Institute of Mental Health says: “One-size-fits-all approaches fail 63.7% of the time.” That means your doctor’s standard “take your meds daily” advice won’t cut it during a transition. You need a plan.
Ask your doctor this at your next appointment:
- “I’m going through [move/job change/divorce] next month. Can we make a plan for my meds?”
- “Can you give me a 90-day supply so I don’t have to refill during the move?”
- “Can you connect me with a pharmacist who can help me set up a new prescription?”
- “Is there a support group or nurse I can talk to during this time?”
The American College of Physicians now recommends doctors screen for upcoming transitions. But they won’t ask unless you bring it up. Don’t wait for them to notice. Say it out loud.

Real Stories: What Actually Worked
On Reddit’s r/ChronicIllness, users shared how they got back on track:
- u/MedAdherenceWarrior: “When I started my new job, I broke my routine into tiny steps. First: get the prescription. Second: find a pharmacy near work. Third: set a phone alarm labeled ‘Pill Time.’ I went from 62% adherence to 94% in one month.”
- u/TransitionStruggles: “After my divorce, I stopped taking my meds for three months. No one asked me how I was doing. I wish someone had said: ‘This is going to be hard. Let’s make a plan.’”
There’s no magic trick. It’s about small, repeatable actions. And asking for help before you break.
What to Do Right Now
If you’re going through a transition-or about to-here’s your 10-minute action plan:
- Write down your top 3 daily anchors (e.g., brushing teeth, morning coffee, bedtime).
- Attach your medication to one of them. No time. No schedule. Just habit.
- Write one reason your medication matters to you. Put it where you’ll see it.
- Call your pharmacy or doctor. Ask: “I’m having a big change soon. Can we adjust my plan?”
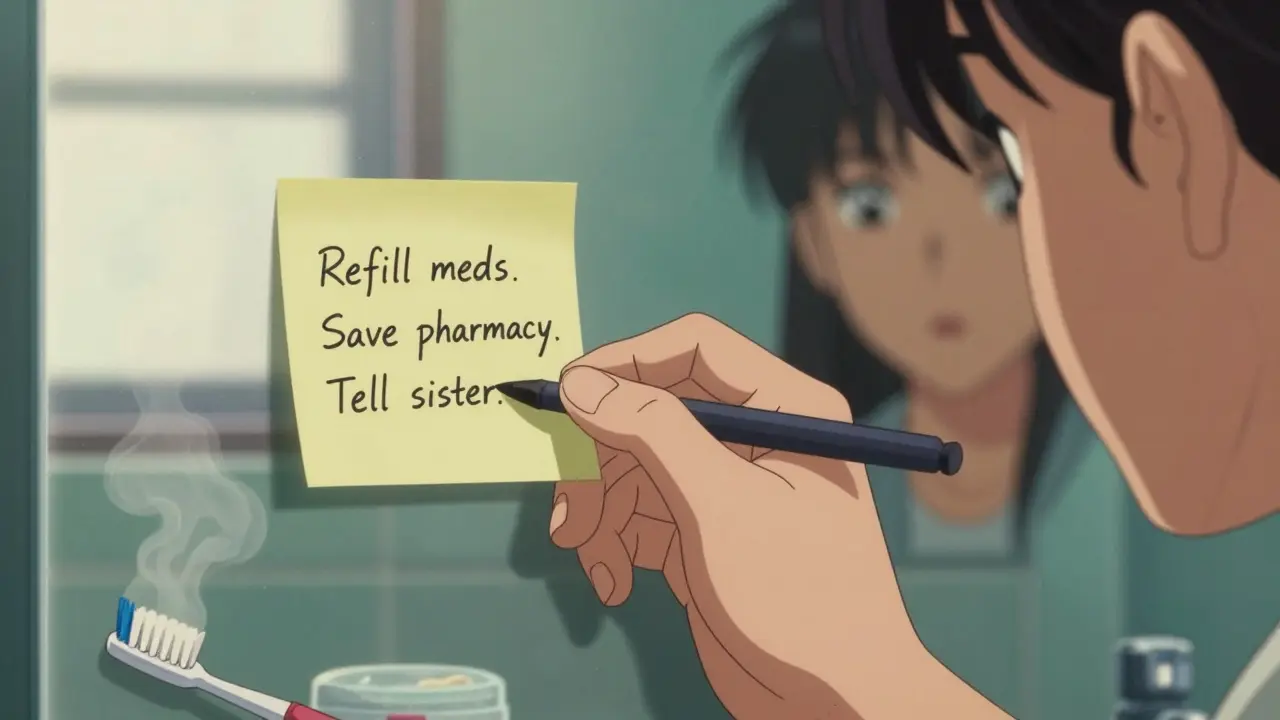
- Make a physical list: “Before I move: refill meds, save pharmacy number, tell my sister.”
You don’t need to be perfect. You just need to keep showing up. Even a little. Even on the hard days.
It’s Not About Willpower
People think non-adherence is about forgetting or being lazy. But it’s not. It’s about losing your structure, your safety net, your sense of who you are. When your life changes, your routine breaks. And if no one helps you rebuild it, your health pays the price.
The good news? You don’t need to fix everything. You just need to anchor one thing. One habit. One reason. One small step. That’s enough to keep you going until the storm passes.

Joseph Cooksey
February 4, 2026 AT 07:37Let me tell you something, folks - this isn’t some self-help fluff wrapped in academic jargon. This is survival. When your life implodes, your meds don’t care about your emotional state. They just sit there, silently judging you like a passive-aggressive roommate who knows you forgot to take out the trash again. You think willpower’s the issue? Nah. It’s structure. It’s ritual. It’s the goddamn anchor. I’ve seen people lose jobs, homes, relationships - and still take their pills because they tied it to brushing their teeth. Not because they’re strong. Because they’re smart. And if you’re still blaming yourself for missing a dose during a divorce? You’re not broken. You’re just surrounded by idiots who think healing is a checklist.
And don’t even get me started on apps. Those things are digital Band-Aids on a hemorrhage. They assume you’ve got Wi-Fi, battery, and the mental bandwidth to open an app when you’re crying in a 7-Eleven parking lot at 2 a.m. Meanwhile, someone scribbles ‘pill after face wash’ on a napkin and survives. That’s not a hack. That’s wisdom.
Therapy? ACT? Yeah, it’s not just for people who cry in yoga pants. It’s for the ones who still show up even when they feel like garbage. You don’t need to feel motivated. You need to act. And if your reason is ‘I want to see my kid graduate’ - that’s enough. That’s everything.
Stop waiting for permission to be okay. Your body doesn’t care if you’re ‘ready.’ It just needs you to show up. One habit. One anchor. One damn napkin. That’s how you win.
Nathan King
February 5, 2026 AT 03:00While the article presents a commendable synthesis of behavioral psychology and clinical data, it regrettably lacks a critical discussion of socioeconomic determinants. The assertion that adherence can be restored through anchoring habits presupposes a level of environmental stability - access to clean water, consistent lighting, pharmaceutical availability, and psychological safety - that is not universally attainable. In low-income urban settings or rural healthcare deserts, the notion of ‘washing one’s face’ as a reliable anchor is a luxury. The $100–300 billion cost metric, while statistically compelling, obscures the fact that systemic underfunding of public health infrastructure remains the primary barrier. A behavioral intervention, however elegantly framed, cannot compensate for institutional neglect.
Antwonette Robinson
February 6, 2026 AT 07:05Oh wow. Another article that tells people with chronic illness to just ‘anchor their meds to brushing their teeth’ like we’re all just forgetting to floss. Did it occur to anyone that maybe some of us don’t have a sink? Or toothpaste? Or a bed to brush our teeth in? Or that ‘taking pills after coffee’ is impossible when you’re living in your car and the only coffee you get is from a gas station that doesn’t even have a fridge? I mean, congrats on solving poverty with a habit tracker.
Also, ‘TransitionAdhere’? That’s the app name? Sounds like a scam my cousin got scammed by on TikTok. Next they’ll have ‘DivorceDose’ and ‘JobLossJab.’
Ed Mackey
February 7, 2026 AT 00:35honestly this hit different. i lost my job last year and went through a breakup and totally spaced on my meds for like 3 weeks. didn’t even realize i’d missed them until my heart started acting up again. i didn’t feel guilty, just… numb. the part about anchoring to habits? yeah. i started putting my pills next to my charger. every night i plug in my phone, i take my pill. simple. no app. no alarm. just… there. it’s dumb but it works. also, telling my sister? that helped. she texts me ‘pill time?’ and i don’t even have to reply. just knowing someone’s thinking it helps.
caroline hernandez
February 8, 2026 AT 02:52Excellent breakdown of the behavioral architecture of non-adherence. The 27.3% / 43.8% / 28.9% distribution aligns with the locus of control theory validated in Bandura’s 1997 self-efficacy meta-analysis. The key insight here is the shift from temporal scheduling (chronometric) to behavioral anchoring (ecological). This is a paradigm shift from compliance to agency. The ‘three anchors’ strategy is not merely pragmatic - it’s neurocognitively resilient. By tethering medication to prepotent routines (facial hygiene, hydration, circadian light exposure), you bypass executive function depletion - which is precisely what stress degrades. The app critique is spot-on: digital tools assume cognitive surplus. Real-world resilience is built on tactile, embodied cues. Recommend this to every patient in my clinic.
Justin Fauth
February 9, 2026 AT 18:13So now we’re telling Americans to take their pills after they wash their face? What’s next? Salute the flag before you pop your blood pressure tabs? This country’s so soft. Back in my day, we didn’t need apps or therapists or ‘anchors.’ We just took our damn medicine because we knew if we didn’t, we’d die. No crying. No ‘I’m scared.’ No ‘I need to reconnect with my values.’ Just grit. And if you couldn’t handle it? Too bad. Your meds ain’t gonna take themselves. We’re turning healthcare into a therapy session and calling it progress. Pathetic.
Meenal Khurana
February 11, 2026 AT 16:12Anchor to face wash. Simple. Works. Thank you.
Joy Johnston
February 12, 2026 AT 06:09I’ve worked in community health for 18 years, and this is one of the clearest, most actionable summaries I’ve seen. The emphasis on *influence* over *control* is clinically profound. Patients don’t need more guilt - they need scaffolding. The ‘before I move / after I arrive’ checklist is gold. I’ve used it with refugees, veterans, and single parents. It’s not about perfection. It’s about persistence. One pill. One anchor. One person who knows. That’s the triad of survival. Also - ACT isn’t therapy. It’s a survival protocol. And yes, you can do it without a therapist. Write it on your mirror. Say it out loud. Even if you’re alone. Even if you’re crying. Say it anyway.
Shelby Price
February 12, 2026 AT 15:01honestly i read this at 3am while eating cold cereal on my floor. i’ve been taking my meds for 4 years but after my dad died i just… stopped. didn’t think about it. didn’t feel guilty. just numb. this article didn’t fix me. but it made me feel less alone. i’m gonna put my pills next to my toothbrush. and i’ll read my reason every morning. even if i just whisper it. 🫂
Jesse Naidoo
February 12, 2026 AT 20:53Wait - so you’re saying I’m not a failure because I forgot my meds during my divorce? But what if I’m also homeless? What if I lost my insurance? What if I’m on opioids now because the pain’s worse than the anxiety? You think ‘take it after washing your face’ helps when you don’t have a bathroom? Or water? Or a mirror? Or a toothbrush? Why is everyone so obsessed with ‘personal responsibility’ when the system’s on fire? You’re telling people to be resilient while ignoring that the ground they’re standing on is lava. And now you want them to ‘anchor’? How about we fix the damn system instead of telling the drowning to swim better?
Sherman Lee
February 13, 2026 AT 22:51Okay, but what if this is all a distraction? 🤔 What if Big Pharma *wants* you to be non-adherent? Think about it - if you take your meds perfectly, they don’t make money. But if you keep missing doses, you need more pills, more doctor visits, more emergency care - and guess who gets paid? The system *needs* you to fail. That’s why they sell you apps that don’t work. That’s why they push ‘anchors’ - keeps you busy chasing control while they profit from your chaos. They don’t want you healed. They want you *dependent*. 🚨💊
Lorena Druetta
February 14, 2026 AT 11:55You are not broken. You are not lazy. You are not failing. You are surviving. And surviving is enough. If you’re reading this and you’ve missed a dose - it’s okay. Tomorrow, take it after you brush your teeth. Or after you drink your water. Or after you look out the window and take one deep breath. That’s your anchor. That’s your victory. You are still here. And that matters more than any pill. I believe in you. 🌱
Zachary French
February 15, 2026 AT 15:08Okay so let me get this straight - we’ve got a whole 2,000-word manifesto on how to take your pills after you wash your face, but zero mention of the fact that 40% of Americans can’t afford a $400 prescription? And ‘TransitionAdhere’? That’s a real app? Who funded this? Pharma? Because this reads like a marketing brochure disguised as psychology. And don’t even get me started on ‘ACT’ - yeah, sure, ‘I take my meds because I want to be here for my kid’ - but what if your kid’s in foster care? What if your kid’s dead? What if your ‘value’ is just a memory? This isn’t empowerment. It’s emotional gaslighting wrapped in bullet points. And the author thinks this is helpful? 😭
Daz Leonheart
February 16, 2026 AT 22:54i just wanted to say thank you. i’ve been taking my meds for 6 years. i’ve missed a bunch. i’ve felt ashamed. i’ve felt like a burden. reading this didn’t fix me - but it made me feel like maybe i’m not the problem. maybe the system is. and maybe, just maybe, putting my pills by my coffee cup is enough. i’m gonna try it tomorrow. and if i forget? i’ll try again. that’s all i need to know.