Storing medications in a shared living space isn’t just about keeping pills out of reach-it’s about keeping them effective, safe, and accountable. Whether you’re living with roommates, adult children, aging parents, or in a group home, poor medication storage can lead to accidental overdoses, spoiled drugs, or even theft. The good news? With a few practical steps, you can eliminate most risks without turning your home into a clinic.
Why Medication Storage Matters More Than You Think
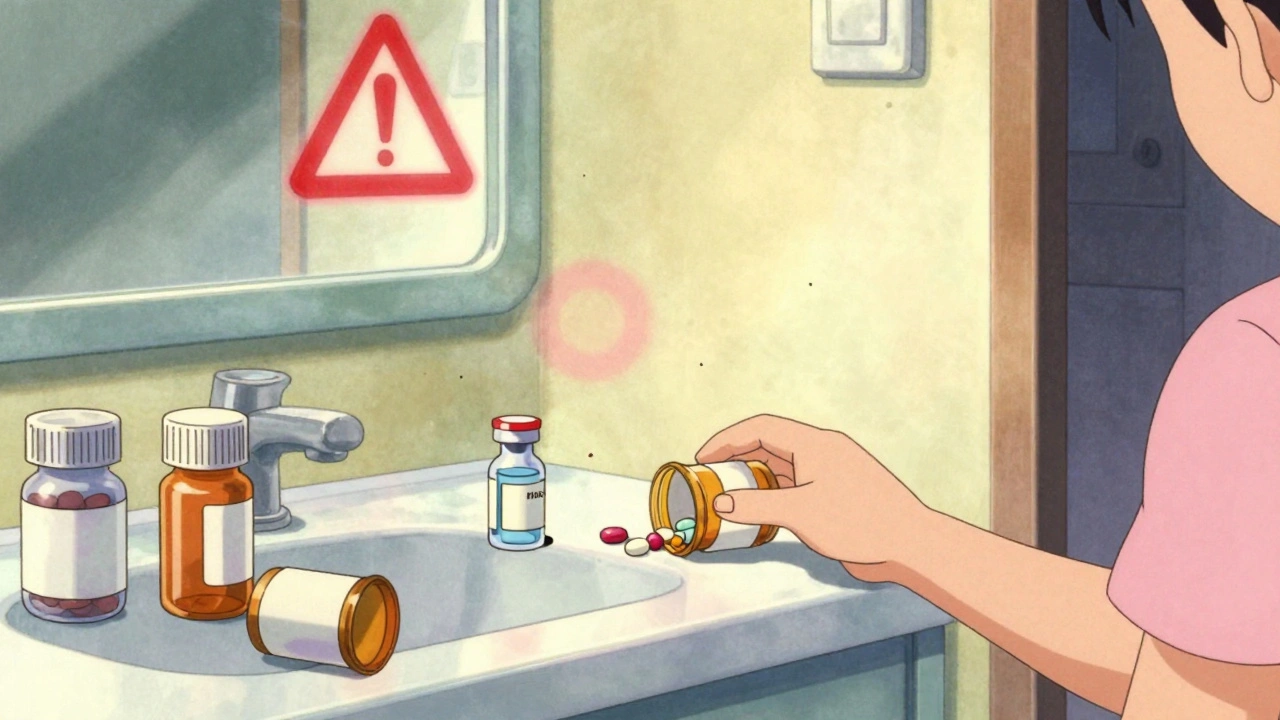
Medications aren’t like snacks or shampoo. A pill left on a bathroom counter can be grabbed by a curious grandchild. Insulin stored on a fridge door can lose potency in days. Antibiotics exposed to heat might stop working entirely. According to the Joint Commission, 13% of healthcare facilities received citations for improper medication storage between 2020 and 2021. That’s not just a rulebook issue-it’s a safety crisis. In multi-generational homes, the stakes are even higher. A 2025 survey by SeniorHelpers found that 67% of families reported at least one medication-related incident in the past year. Nearly half of those involved children accessing meds stored in unlocked cabinets. And it’s not just kids. People with dementia, substance use disorders, or cognitive impairments are at risk too. The solution isn’t complexity-it’s clarity. You don’t need a locked room or a nurse on staff. You need a system.Step 1: Take Stock of Everything
Start by gathering every pill, liquid, patch, and inhaler in the home. This includes:- Prescription drugs
- Over-the-counter painkillers (ibuprofen, acetaminophen)
- Vitamins and supplements
- Topical creams and ointments
- Insulin, epinephrine pens, or other injectables
Step 2: Sort by Storage Needs
Not all meds need the same conditions. Group them into three categories:- Room temperature: Most pills and capsules. Store in a cool, dry place away from sunlight-like a bedroom drawer, not the bathroom.
- Refrigerated: Insulin, some antibiotics, eye drops, and biologics. Must be kept between 36-46°F. The center shelf of the fridge is the most stable spot. Never store on the door.
- Controlled substances: Opioids, benzodiazepines, stimulants. These require a locked container, no exceptions.
Step 3: Choose the Right Storage Solution
Forget using a junk drawer. You need dedicated storage. Here’s what works:- Locked medicine cabinet: Ideal for room-temperature meds. Look for ones with key locks or digital codes. Avoid glass-front cabinets-kids can break them.
- Medication safe: A small, fire-resistant safe (like those used for jewelry) works great for controlled substances. Some models even alert you if opened at odd hours.
- Locked drawer in a bedroom: Best for households without a central cabinet. Assign one drawer per person. Label it clearly.
- Dedicated fridge compartment: If you store insulin or other cold meds, use a small, labeled container inside the fridge. Put it on the center shelf and tape a note: “MEDICATIONS ONLY-NO FOOD.”

Step 4: Label Everything Clearly
Mislabeling is a leading cause of errors. Every container must have:- Full name of the person it’s for
- Drug name and dosage
- Time and frequency of use
- Prescribing doctor’s name
Step 5: Control Access
Only people who need to take the meds-or help administer them-should have access. That means:- Keys or codes are given only to responsible adults
- Children and teens are not trusted with access, even if they’re responsible
- Visitors don’t know where the meds are stored
Step 6: Keep Records (Even at Home)
You don’t need a full medical chart, but you do need a simple log. Keep a notebook or digital note with:- Each person’s meds
- When they’re taken
- Any side effects or missed doses
Step 7: Train Everyone Who Lives There
This is the part most people skip. You can have the best safe in the world, but if your teenager thinks “pain pills are just for headaches,” you’re asking for trouble. Hold a 10-minute family meeting. Show where meds are stored. Explain why they’re locked. Say plainly: “This isn’t about trust-it’s about safety.” If someone has dementia or memory issues, use visual cues. A photo of the locked drawer with a red sticker saying “MEDS” helps more than a verbal reminder. SeniorHelpers launched a free medication safety certification for caregivers in April 2025. Over 12,500 people completed it in the first month. You don’t need a certificate-but you do need to be clear.
What Not to Do
Avoid these common mistakes:- Storing meds in the bathroom-humidity ruins them
- Leaving pills on nightstands-easy to grab by accident
- Using original pill bottles without labels-what’s this pill for again?
- Keeping old meds “just in case”-they expire, and they’re a risk
- Sharing prescriptions-never, ever do this
Special Cases: Insulin, Epinephrine, and Controlled Substances
Some meds need extra care:- Insulin: Must stay cold. If it gets too hot, it breaks down. Always store in the center of the fridge. Never freeze.
- Epinephrine pens (EpiPens): Keep at room temperature. Don’t refrigerate. Store where they can be grabbed fast in an emergency-like a bedside drawer, not a locked safe.
- Controlled substances (oxycodone, Adderall, Xanax): Locked container only. No exceptions. Consider a smart lock that texts you if opened.
What to Do If Something Goes Wrong
Accidents happen. If a child swallows a pill, or someone takes the wrong dose:- Call Poison Control immediately (1-800-222-1222 in the U.S.)
- Have the medication bottle ready-name, dose, time taken
- Don’t wait for symptoms. Act fast.
Final Thought: It’s Not About Control-It’s About Care
Medication storage isn’t about being strict. It’s about being smart. You’re not trying to spy on your roommate or control your parent. You’re protecting everyone in the home-from toddlers to seniors-from harm. The data doesn’t lie: locked storage cuts incidents by more than half. Proper refrigeration keeps drugs working. Clear labels prevent mistakes. And a simple log? It’s the difference between chaos and calm. Start small. Pick one thing today: empty the bathroom cabinet. Put the insulin in the center of the fridge. Lock the painkillers. That’s enough. Do one thing right-and build from there.Can I store my medications in the bathroom cabinet?
No. Bathrooms are too humid and warm, which can damage pills, liquids, and patches. Moisture causes medications to break down faster, making them less effective or even unsafe. Always store meds in a cool, dry place like a bedroom drawer or locked cabinet away from showers and sinks.
What’s the best way to store insulin in a shared fridge?
Store insulin on the center shelf of the refrigerator, where temperatures are most stable (36-46°F). Never put it on the door, as that area fluctuates in temperature. Use a small, clearly labeled container marked “INSULIN ONLY - NO FOOD” to prevent accidental disposal or contamination.
Do I need a locked cabinet if I live alone with my elderly parent?
Yes. Even in a two-person home, locked storage is critical. Cognitive decline, memory issues, or accidental confusion can lead to overdoses. A simple locked drawer or small safe prevents mistakes. The Joint Commission recommends locking all controlled substances and strongly advises it for all medications in shared environments.
How do I know if my medication has gone bad?
Check the expiration date first. Then look for changes: pills that are discolored, crumbly, or have an odd smell; liquids that are cloudy or have particles; patches that are sticky or faded. If in doubt, throw it out. The FDA says degraded medications can be ineffective or harmful. When in doubt, contact your pharmacist.
What should I do with expired or unused medications?
Never flush them down the toilet or throw them in the trash without mixing. The safest way is to use a drug take-back program. Many pharmacies and police stations offer free drop-off bins. If none are nearby, mix pills with coffee grounds or cat litter, seal them in a bag, and throw them in the trash. Remove personal info from bottles first.
Are smart medication safes worth the cost?
If someone in your home has a history of substance misuse, dementia, or frequent missed doses, yes. Smart safes with temperature monitoring, access logs, and alerts can prevent emergencies. They cost $100-$300, but they’re far cheaper than an ER visit. Models from DosePacker and others are already used in over 100 care facilities across the U.S.
Neelam Kumari
December 10, 2025 AT 14:10Doris Lee
December 11, 2025 AT 01:44Taylor Dressler
December 12, 2025 AT 16:28Also, never flush meds. Ever. That’s how we get pharmaceuticals in drinking water. Mix with coffee grounds. Seal. Trash.
Jean Claude de La Ronde
December 14, 2025 AT 13:44Rebecca Dong
December 14, 2025 AT 23:20Nikki Smellie
December 15, 2025 AT 17:29Sylvia Frenzel
December 17, 2025 AT 13:35Queenie Chan
December 18, 2025 AT 05:20Also, I just labeled my vitamins with neon stickers. ‘B12 - DO NOT TOUCH - KAITLYNN’S SOUL ENHANCER.’ It’s art.
Stephanie Maillet
December 19, 2025 AT 09:08Maybe the real solution isn’t the lock-it’s the conversation. The 10-minute meeting. The ‘I’m scared for you’ talk. The one that doesn’t come with a checklist.
Michaux Hyatt
December 20, 2025 AT 17:48Raj Rsvpraj
December 22, 2025 AT 17:15Mia Kingsley
December 24, 2025 AT 09:35Ariel Nichole
December 25, 2025 AT 02:34Kaitlynn nail
December 25, 2025 AT 05:28Courtney Blake
December 25, 2025 AT 15:40