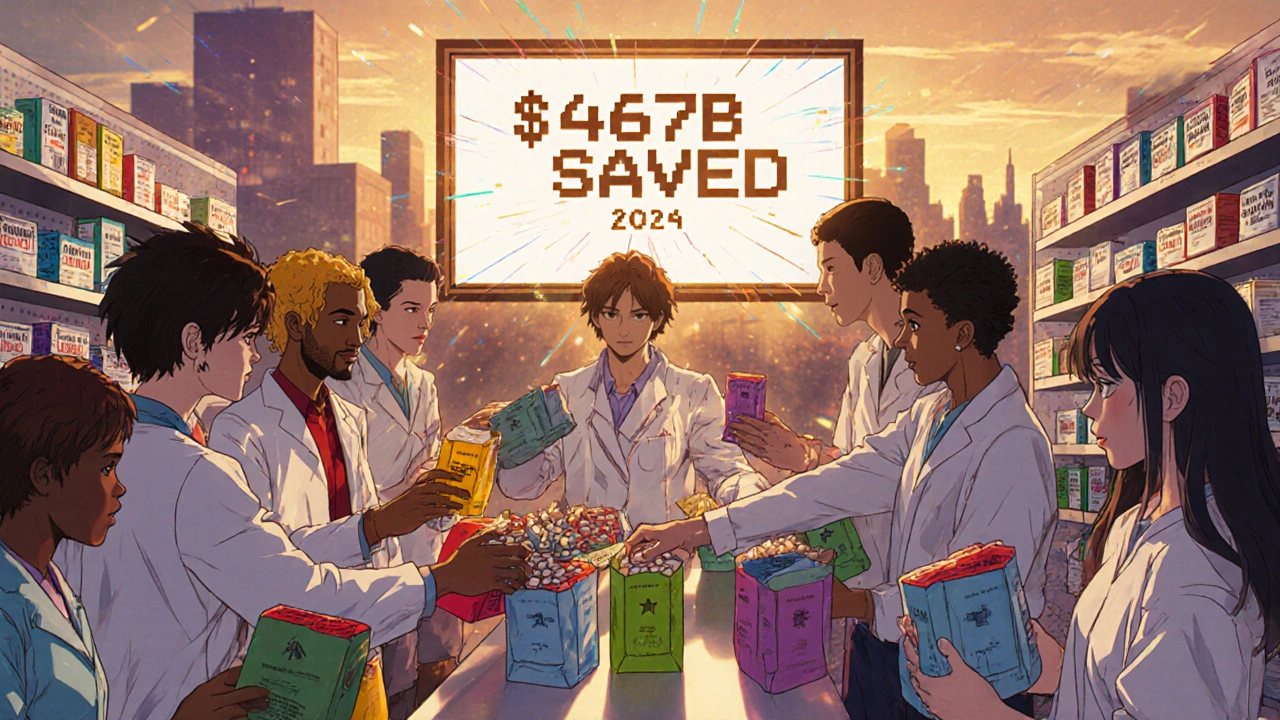
Every year, Americans spend nearly half a trillion dollars less on prescription drugs because of generic medications. That’s not a guess. It’s a fact backed by hard numbers: in 2024 alone, generic and biosimilar drugs saved the U.S. healthcare system $467 billion. Over the last decade, those savings added up to $3.4 trillion. That’s more than the entire GDP of Canada or Australia. And it’s all because of pills and injections that cost a fraction of their brand-name counterparts.
How Do Generics Save So Much Money?
The math is simple: 90% of all prescriptions filled in the U.S. are for generic drugs. But those same generics make up only 12% of total drug spending. In 2024, patients paid $98 billion for generics. They paid $700 billion for brand-name drugs. That’s a 700% difference in cost for the same active ingredients. The reason? Generic manufacturers don’t have to repeat expensive clinical trials. They just need to prove their version works the same way as the original. That cuts development costs dramatically. Once a brand-name drug’s patent expires, multiple generic companies jump in. Competition drives prices down. For example, the generic version of Lipitor (atorvastatin) dropped from $120 a month to under $10 within a year of patent expiration. Some generics now cost less than a cup of coffee. Biosimilars-generic versions of complex biologic drugs like Humira or Enbrel-are adding even more savings. In 2024, biosimilars saved $20.2 billion in just one year. Since 2015, they’ve saved $56.2 billion total. These drugs used to cost $20,000 a year. Now, some biosimilars cost under $5,000.Who’s Really Saving Money?
It’s not just patients. The biggest savings go to public programs. In 2024, generics saved Medicare $142 billion and Medicaid $62.1 billion. That’s money that could pay for nursing home care, mental health services, or even expand coverage to millions more people. Private insurers saved too. Express Scripts, one of the largest pharmacy benefit managers, reported $18.3 billion in savings in 2023 just from switching patients to generics. Blue Cross Blue Shield estimates that if pay-for-delay deals-where brand companies pay generics to stay off the market-were banned, the system could save $12 billion a year. Even small savings add up fast. A patient on a $150-a-month brand drug who switches to a $3 generic saves $1,440 a year. Multiply that by millions of people, and you get a trillion-dollar impact.Top Generics Driving the Savings
Not all generics are created equal. The biggest savings come from drugs used to treat the most common chronic conditions:- Metformin (for type 2 diabetes) - saved $11.3 billion in 2023
- Atorvastatin (Lipitor generic) - saved $10.9 billion
- Levothyroxine (for hypothyroidism) - saved $9.8 billion
- Amlodipine (for high blood pressure) - saved $8.7 billion
- Omeprazole (for acid reflux) - saved $7.6 billion
Why Are Some Patients Still Paying Too Much?
Despite the savings, many people still struggle to afford prescriptions. Why? Because the system isn’t designed to pass savings on to patients. Pharmacy Benefit Managers (PBMs) control which drugs are covered and at what price. Many still push brand-name drugs-even when generics are cheaper-because they get bigger rebates from manufacturers. A 2023 survey found that 42% of patients skipped doses or didn’t fill prescriptions because of cost. But among those who switched to generics, 89% said they were happy with the results. Another problem: some Medicare Part D plans still list brand drugs as preferred, even when generics are available. Patients end up paying more because their plan doesn’t incentivize the cheaper option. And then there’s the “formulation myth.” Some patients swear their brand drug works better. But studies show generic drugs are just as effective. A Drugs.com analysis of over 15,000 reviews found that 87% of users rated cost as excellent, but only 63% rated effectiveness the same. That gap suggests perception, not reality, is driving resistance.Barriers to Even More Savings
The system was supposed to be simple: patent expires → generics enter → prices drop. But big pharma has found loopholes. One tactic is “patent thickets”-filing dozens of minor patents to block generics. A 2024 JAMA study found that just four drugs used patent thickets to delay generics, costing the system over $3.5 billion in two years. Another is “product hopping”: changing a drug’s form (like switching from a pill to a liquid) just before the patent expires, forcing patients to restart treatment on the new version. This resets the clock on generic competition. The FDA approved 1,145 generic drugs in 2024, but many face delays because of “citizen petitions”-baseless complaints filed by brand companies to slow approval. There were 118 such petitions between 2018 and 2023. Even state policies vary. California forces pharmacies to substitute generics unless the doctor says no. Result? 98% generic use. Texas lets pharmacists choose. Result? 87% use. The difference? Billions in lost savings.
What’s Next for Generic Savings?
The future looks bright. The FDA has already approved $14 billion in new generic drugs, with another $24 billion in pipeline drugs expected by 2025. These include complex generics like inhalers and injectables-drugs that used to cost $1,000 a month and are now dropping to $200. Biosimilars are accelerating too. With more drugs becoming “interchangeable” (meaning pharmacists can swap them without doctor approval), savings will grow faster. The market is growing at 22.7% per year. Legislation like S.1041-the Affordable Prescriptions for Patients Act-could add $7.2 billion in annual savings by cracking down on patent abuse. It passed the Senate committee with bipartisan support. But there’s a risk: consolidation. The top 10 generic manufacturers now control 63% of the market, up from 51% in 2015. Fewer competitors mean less pressure to lower prices. And drug shortages-287 generic medications were in short supply as of December 2024-can spike prices overnight.What You Can Do
If you’re paying for prescriptions:- Always ask your doctor: “Is there a generic version?”
- Use GoodRx or SingleCare to compare prices at local pharmacies.
- Ask your insurer why they’re not covering the generic.
- If your plan forces you to use a brand, file an appeal.
Why This Matters Beyond the Wallet
Healthcare spending in the U.S. hit $4.9 trillion in 2023. Prescription drugs made up $490 billion of that. Generics kept that number from being $1.2 trillion. Without generics, more people would skip medications. More would go into emergency rooms. More would file for bankruptcy. The savings aren’t just numbers-they’re people staying out of hospitals, keeping their jobs, and living longer. As Dr. A. Mark Fendrick put it: “Leveraging generics is the only way we can afford the next breakthrough.” The system isn’t perfect. But right now, generic drugs are the most powerful tool we have to make healthcare affordable. And they’ve already saved trillions.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for quality, purity, and performance. Studies show generics work just as well in treating conditions like high blood pressure, diabetes, and depression. The perception that they’re less effective often comes from differences in inactive ingredients (like fillers or dyes), which don’t affect how the drug works in the body.
Why do some pharmacies charge more for generics than others?
Pharmacy pricing varies because of how Pharmacy Benefit Managers (PBMs) negotiate deals with manufacturers. Some pharmacies get better discounts, while others are locked into higher prices. Also, some pharmacies use generics as loss leaders to attract customers. Using tools like GoodRx or SingleCare can help you find the lowest price-sometimes as low as $4 for a 30-day supply. Cash prices are often cheaper than insurance copays.
Can I trust generic drugs made overseas?
Yes. Over 80% of generic drugs sold in the U.S. are manufactured overseas, mostly in India and China. But every facility-whether in the U.S., India, or elsewhere-must pass the same FDA inspections. The FDA conducts thousands of inspections each year. A drug made in India is held to the same standard as one made in New Jersey. The location doesn’t determine quality; the inspection record does.
Why do some doctors still prescribe brand-name drugs?
Some doctors prescribe brands out of habit, or because they’re influenced by pharmaceutical reps. Others may be unaware of generic availability. In rare cases, a patient may have a sensitivity to an inactive ingredient in the generic version. But for 95% of prescriptions, there’s no medical reason to avoid generics. Always ask: “Is there a generic alternative?” and “Why are you recommending this brand?”
How do biosimilars differ from regular generics?
Biosimilars are generic versions of biologic drugs, which are made from living cells (like proteins). Unlike small-molecule generics, biosimilars can’t be exact copies because biologics are too complex. Instead, they must be “highly similar” with no clinically meaningful differences. They’re more expensive to develop than regular generics, but still cost 15-35% less than the original. They’ve already saved over $56 billion since 2015 and are expected to save even more as more become interchangeable.
What’s stopping us from saving even more money with generics?
Three main things: patent abuse (like filing dozens of minor patents to delay generics), pay-for-delay deals (where brand companies pay generics to stay off the market), and administrative barriers like prior authorization requirements. These tactics extend monopolies and keep prices high. Legislative action, like the Affordable Prescriptions for Patients Act, aims to fix these issues. Until then, savings will continue to be held back.
Bailey Sheppard
November 17, 2025 AT 17:33Generics are the unsung heroes of American healthcare. I’ve been on metformin for years and never even thought twice about switching from brand to generic-until I saw the price difference. Now I feel kinda dumb for ever doubting it. These pills save lives, not just money.
steffi walsh
November 18, 2025 AT 10:24OMG YES!! 🙌 I switched my mom to generic Lipitor last year and she’s been saving $100/month. She cried when she saw the receipt. People don’t realize how much this stuff matters-until it’s their own prescription. Generics = dignity.
Yash Nair
November 20, 2025 AT 08:45India makes most of these generics and still u guys act like its magic. We make them cheaper because we dont pay 10k for a PhD to write a 3 line patent. US system is broken not the drugs. Also stop pretending generics are new. We’ve been doing this since 1980s.
Conor McNamara
November 21, 2025 AT 07:41they say generics are the same... but have u ever noticed how the pill looks diffrent? same color, same shape, same lettering... but somehow it dont work the same. i think the gov is hiding somethin. why do they even let the pills look diffrent if theyre the same? something dont add up.
Leilani O'Neill
November 22, 2025 AT 13:00Of course generics save money. But let’s not pretend this is some moral victory. The U.S. is a nation of consumers who refuse to pay for quality. We’ve turned medicine into a discount aisle at Walmart. And now we’re shocked when people skip doses? Pathetic.
Riohlo (Or Rio) Marie
November 24, 2025 AT 04:11Let’s be real-the real villains aren’t the generic manufacturers. They’re the PBMs who pocket the rebates while patients get stuck with $50 copays for a $3 pill. It’s not about generics failing. It’s about the system being rigged by middlemen who don’t give a damn if you die or not.
Girish Pai
November 26, 2025 AT 02:41Generic penetration rate is at 90% but market share is 12%-this is textbook oligopoly suppression. The structural inefficiency lies in the patent evergreening ecosystem and the rent-seeking behavior of brand incumbents. We need structural reform, not just consumer education.
Louie Amour
November 27, 2025 AT 08:26You think this is about savings? Nah. It’s about control. The FDA approves generics but then the insurance companies force you to use the ones they’ve partnered with. And if you ask why? They’ll say ‘it’s cheaper.’ But you’re still paying more than you should. It’s all a game. And you’re not even in the room.
Kristi Joy
November 28, 2025 AT 18:22My sister was on a $200 brand-name antidepressant. Switched to generic-same effect, same side effects, $4 a month. She said it was the first time in years she felt like she could breathe. This isn’t about money. It’s about access. And we owe it to every person who can’t afford to be sick to keep fighting for this.
Denny Sucipto
November 29, 2025 AT 00:11My grandma used to say, ‘if it works, it works.’ She took generics for 20 years. Never had a problem. People worry about the color of the pill like it’s magic. Nah. It’s chemistry. And chemistry doesn’t care who made it.
Hal Nicholas
November 29, 2025 AT 17:38They’re gonna tell you biosimilars are ‘just like generics.’ But they’re not. They’re expensive, complicated, and half the time, the doctors don’t even know how to prescribe them. And now they’re trying to make pharmacists swap them without telling you? That’s not progress. That’s a trap.
Shilpi Tiwari
December 1, 2025 AT 00:16Generic drug manufacturing in India? Yeah, and they’re the ones who kept the world supplied during COVID. We’re not talking about some shady back-alley lab. We’re talking about FDA-certified facilities with ISO standards. The U.S. can’t even produce its own syringes anymore. So shut up and thank them.