Calcium Intake Calculator
Daily Calcium Calculator
Track your calcium intake from foods mentioned in the article. Recommended daily intake: 1,000 mg for adults, 1,200 mg for adults over 70.
Your Daily Calcium Intake
0 mg of calcium
Ever wondered why your dentist sometimes talks about bone health while you’re sitting in the chair? The link between the minerals that build your skeleton and the health of your smile is stronger than you might think. This guide walks you through what happens when you don’t get enough calcium, how it shows up in your mouth, and practical steps to keep both your bones and teeth in shape.
What is calcium deficiency?
Calcium deficiency is a condition where the body lacks sufficient calcium to support bone development, muscle function, and nerve signaling. Without enough calcium, the body pulls the mineral from its reserves - mainly the bones - to keep vital processes running. Over time, that borrowing weakens the skeleton and can spill over into the structures that protect your teeth.
Why your teeth need calcium
The outer layer of each tooth, called tooth enamel is the hardest substance in the human body, made mostly of a crystal form of calcium phosphate. Enamel doesn’t repair itself, so it relies on a steady supply of calcium during the formation stage and to resist acid attacks later on. Below the enamel, the dentin and the supporting alveolar bone also depend on calcium to stay dense and resilient.
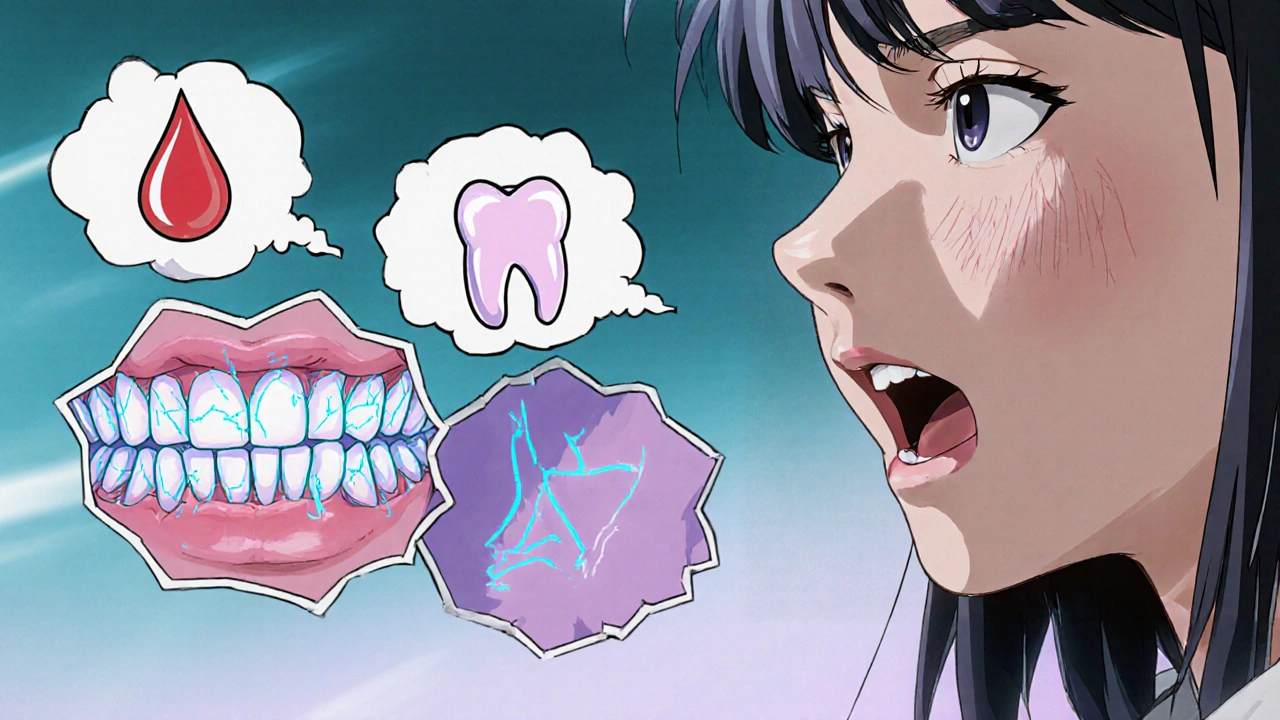
Signs that low calcium is hurting your mouth
- Frequent tooth sensitivity, especially to cold or sweet foods.
- Enamel chips or cracks that seem to happen more easily.
- Bleeding gums or rapid plaque buildup, indicating periodontal disease is an inflammation of the gums and supporting bone that can lead to tooth loss if untreated.
- Unexplained jaw pain or a feeling of looseness in the teeth.
If any of these symptoms sound familiar, a quick calcium check could be the first clue.
How common is calcium deficiency?
Studies from the UK Nutrition Survey in 2024 show that about 25% of adults aged 45 and older have blood calcium levels below the recommended range. Women, especially post‑menopausal, and people with limited dairy intake are at higher risk. Even younger adults who follow strict vegan or low‑calorie diets can end up short on calcium if they don’t plan their meals carefully.
Boosting calcium for better dental health
Adding calcium back into your diet doesn’t have to be a chore. Here are some tasty ways to hit the target:
- Drink a glass of milk is a dairy product that provides roughly 125 mg of calcium per 100 ml daily. If you’re lactose‑intolerant, fortified plant milks work just as well.
- Snack on calcium‑rich foods like cheese, yogurt, or sardines with bones. A small serving of cheddar can give you about 200 mg of calcium.
- Include leafy greens such as kale, collard greens, and bok choy. They deliver calcium without the saturated fat found in some animal sources.
- Consider a calcium supplement if you struggle to meet the 1,000 mg daily recommendation. Choose one with vitamin D, which helps the body absorb calcium more efficiently.

Other factors that work hand‑in‑hand with calcium
Calcium isn’t a solo player. A handful of companions help lock it into place and protect your teeth:
- Vitamin D is a fat‑soluble vitamin that boosts calcium absorption from the gut. Sunlight exposure for 10‑15 minutes a day, or a modest supplement, can keep levels healthy.
- Fluoride, found in most public water supplies and toothpaste, strengthens enamel by forming a more acid‑resistant mineral layer.
- Good oral hygiene - brushing twice daily, flossing, and regular dental check‑ups - reduces plaque, the main driver of enamel erosion.
- Managing osteoporosis is a disease where bones become porous and fragile, often linked to chronic calcium deficiency with weight‑bearing exercise can protect the jawbone that holds your teeth.
When these pieces fall into place, you give your teeth the best chance to stay strong for a lifetime.
Quick reference: Calcium‑rich foods
| Food | Calcium (mg) | Notes |
|---|---|---|
| Milk (whole) | 125 | Also provides vitamin D and protein |
| Cheddar cheese | 720 | High calcium, watch saturated fat |
| Yogurt (plain) | 110 | Contains probiotics for gut health |
| Sardines (with bones) | 382 | Also rich in omega‑3 fatty acids |
| Kale (cooked) | 150 | Low in oxalates, which can block calcium absorption |
| Almonds | 264 | Good snack, but high in calories |
Putting it all together
Think of your mouth as a tiny extension of your skeleton. When calcium levels dip, the first warning signs often appear on your teeth. By checking your diet, adding a reliable source of calcium, and supporting it with vitamin D and good oral care, you can nip problems in the bud. If you’re unsure whether you’re getting enough, a simple blood test can give you a clear picture, and your dentist can run a quick check for enamel health during a routine visit.
Can a calcium supplement replace dairy?
Supplements can fill the gap, but dairy also provides protein, vitamin D, and other minerals that help calcium work better. If you’re vegan or lactose‑intolerant, choose a fortified plant‑based milk and a calcium‑vitamin D combo tablet.
Does low calcium cause cavities?
Calcium itself doesn’t cause cavities, but weak enamel from low calcium makes teeth more vulnerable to acid attacks. Pair calcium‑rich foods with fluoride toothpaste to keep decay at bay.
How much calcium do adults really need?
The UK’s reference intake is about 1,000 mg per day for most adults, rising to 1,200 mg for women over 70. Split the amount across meals for better absorption.
Is calcium linked to gum disease?
Indirectly, yes. Low calcium can weaken the bone that supports the gums, making it easier for periodontal disease to progress. Maintaining calcium levels helps keep that bone strong.
Can I get enough calcium from plant foods alone?
Absolutely. Dark leafy greens, fortified tofu, almonds, and calcium‑enriched plant milks can meet daily needs. Pair them with vitamin D sources to boost absorption.
Ben Bathgate
October 19, 2025 AT 19:37Your post is just a fancy grocery list for teeth.
Ankitpgujjar Poswal
October 19, 2025 AT 22:23Look, you’ve nailed the basics, but let’s fire it up-hit those calcium‑rich foods hard, smash a glass of fortified soy milk daily, and don’t let the fear of dairy hold you back. Your gums will thank you, and your dentist will finally stop nagging.
Christopher Burczyk
October 20, 2025 AT 01:10While the article covers the essentials, it overlooks the biochemical interplay between parathyroid hormone and calcium homeostasis, which is critical for interpreting lab results. A more rigorous examination of serum calcium versus ionized calcium would strengthen the clinical relevance.
Christian Georg
October 20, 2025 AT 03:57Calcium isn’t just a building block for your bones; it’s the quiet hero behind enamel remineralization and the stability of the periodontal ligament. When dietary intake dips, the body taps into skeletal reserves, subtly weakening the alveolar bone that supports each tooth. This can manifest as increased sensitivity to cold drinks, a phenomenon many dismiss as "just a toothache." Studies from the UK Nutrition Survey in 2024 show a quarter of adults over 45 have sub‑optimal calcium levels, correlating with higher incidences of early‑stage periodontitis.
One practical tip is to pair calcium sources with vitamin D‑rich foods or sunlight exposure; vitamin D acts like a key, unlocking calcium absorption in the gut. For those avoiding dairy, fortified plant milks, calcium‑set tofu, and canned fish with bones are excellent alternatives, delivering 300‑400 mg per serving.
Another often‑missed factor is the role of fluoride in stabilizing the enamel crystal lattice, making it more resistant to acidic challenges. Using a fluoride toothpaste twice daily creates a protective fluorapatite layer, reducing demineralization risk.
Don’t forget the impact of dietary oxalates-foods like spinach can bind calcium, making it less bioavailable. Cooking and pairing them with vitamin C‑rich foods can mitigate this effect.
Regular dental check‑ups remain vital; dentists can detect early enamel erosions and recommend remineralizing agents such as casein phosphopeptide‑amorphous calcium phosphate (CPP‑ACP) gels.
Lastly, weight‑bearing exercise stimulates bone remodeling, indirectly supporting jawbone density and gum health. Even a modest 30‑minute walk or resistance routine a few times a week can make a difference. :)
Madhav Dasari
October 20, 2025 AT 06:43Imagine your smile as a fortress-each bite of cheese or sip of fortified milk is a brick reinforcing the walls. When those bricks are missing, the enemies-acidic drinks and plaque-storm in with ease. That dramatic crack you felt on a cold soda? It’s the same as a castle wall giving way under siege!
DHARMENDER BHATHAVAR
October 20, 2025 AT 09:30Include a daily portion of leafy greens and a vitamin D supplement; this combo maximizes calcium uptake.
Kevin Sheehan
October 20, 2025 AT 12:17From a philosophical angle, the mouth mirrors the body’s inner balance; neglecting minerals disrupts harmony. Aggressive action on nutrition restores that equilibrium. A mind attuned to health sees teeth as extensions of skeletal integrity.
Jay Kay
October 20, 2025 AT 15:03The article is okay but could use more drama about calcium being the superhero of teeth.
Sarah Unrath
October 20, 2025 AT 17:50i think its good but theres a few typo errors like alot instead of a lot and its missing punctuation
James Dean
October 20, 2025 AT 20:37well its a solid guide the tips are useful but could be shorter
Monika Bozkurt
October 20, 2025 AT 23:23From a clinical perspective, the integration of calcium homeostasis mechanisms with periodontal pathology elucidates the etiological nexus, thereby informing evidence‑based prophylactic protocols. Leveraging fortified nutraceuticals alongside adjunctive fluoride therapies can synergistically augment enamel remineralization kinetics. Moreover, interdisciplinary collaboration between dental practitioners and nutritionists will optimize patient outcomes, particularly in postmenopausal cohorts at elevated osteoporotic risk.