Geriatric Medication Safety Checker
Check Medication Safety for Elderly Patients
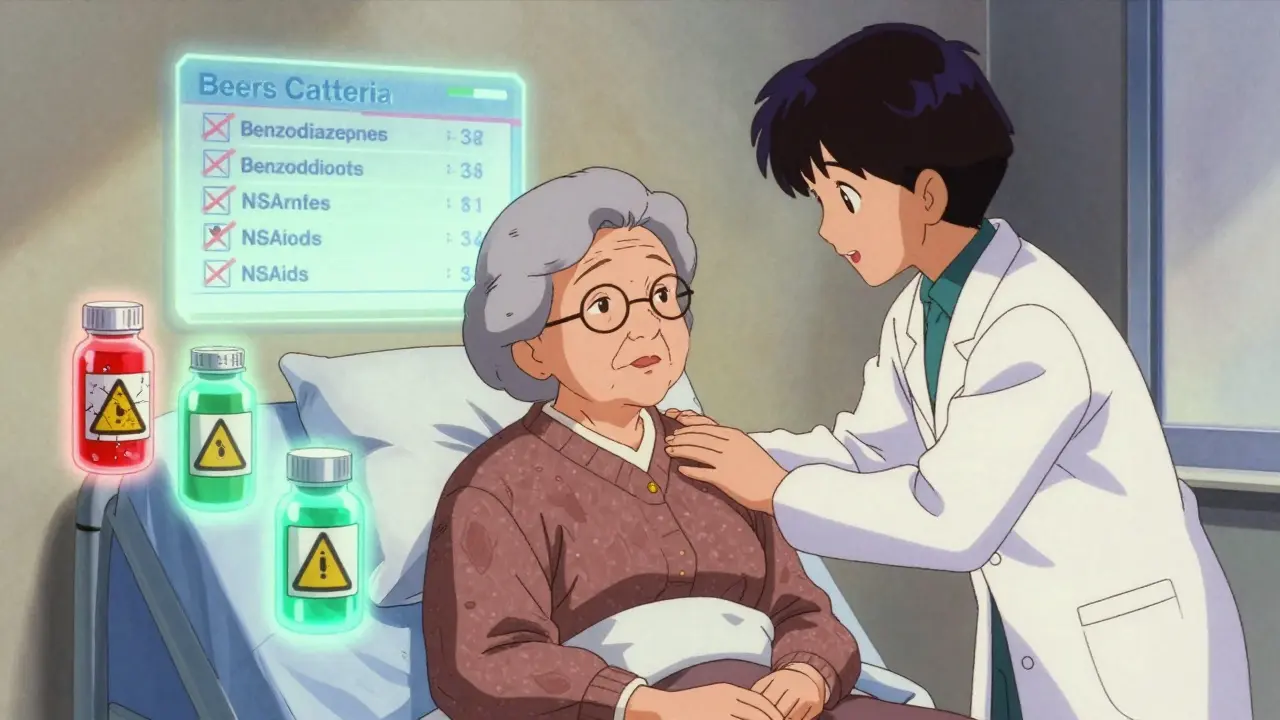
Enter a medication name or category to see if it's potentially inappropriate for patients over 65 based on the Beers Criteria 2023 and Alternatives List 2025.
Every year, over 1 in 3 hospital admissions for people over 65 are caused by medication problems. It’s not just about taking too many pills-it’s about taking the wrong ones. For older adults, even common drugs can trigger falls, confusion, kidney damage, or internal bleeding. The stakes are high, and the solutions are clearer than ever.
Why Older Adults Are at Higher Risk
As we age, our bodies change in ways that make medication use riskier. The liver and kidneys don’t filter drugs as efficiently. Body fat increases while water content drops, meaning drugs like benzodiazepines or antidepressants linger longer in the system. Many older adults take five, ten, or even more medications daily-this is called polypharmacy. And when you stack drugs, the chances of dangerous interactions spike. A 2025 JAMA Network Open review found that seniors prescribed even one potentially inappropriate medication (PIM) are 26% more likely to have an adverse drug event. With two or more PIMs, that risk jumps to over 60%. These aren’t rare outliers-they’re routine. A 72-year-old on a blood thinner, an anticholinergic for overactive bladder, and a NSAID for arthritis? That’s a triple threat. One study showed these combinations lead to emergency room visits 3 times more often than expected.The Beers Criteria: Your Clinical Compass
The American Geriatrics Society (AGS) first published the Beers Criteria in 1991. Since then, it’s become the most cited tool in geriatric care, with over 1,200 research papers referencing it. The 2023 update is the latest version, and it’s more precise than ever. It lists 139 medications or drug classes that should be avoided or used with extreme caution in adults 65+. These aren’t random guesses-they’re based on decades of clinical data. For example:- Tramadol was added because it raises the risk of hyponatremia, especially when taken with SSRIs or diuretics.
- Aspirin for primary heart disease prevention is now discouraged for anyone 70+, not just 80+, due to bleeding risks.
- Indomethacin and ketorolac (strong NSAIDs) are flagged for all older adults-no exceptions.
What’s New: The Alternatives List
In July 2025, the AGS released something groundbreaking: the Beers Criteria® Alternatives List. This isn’t just about what to avoid-it’s about what to use instead. Clinicians have long struggled with deprescribing. You take away a drug, but then what? The Alternatives List answers that. It gives 47 evidence-backed options across 12 categories:- For insomnia: sleep hygiene, cognitive behavioral therapy (CBT-I), melatonin-not benzodiazepines.
- For overactive bladder: timed voiding, pelvic floor exercises-not oxybutynin or tolterodine.
- For chronic pain: physical therapy, acetaminophen (at safe doses), topical capsaicin-not opioids or NSAIDs.
Real-World Successes and Failures
Some hospitals are getting this right. At the Mayo Clinic’s emergency department, a team of pharmacists, geriatricians, and ED doctors cut PIM prescriptions by 38% in six months. How? They redesigned workflows. Pharmacists joined morning rounds. They had direct access to prescribing systems. They didn’t just flag drugs-they offered alternatives. At the University of Alabama at Birmingham, pharmacist-led medication reconciliation cut 30-day readmissions due to drug problems by 22%. But not every program works. In one survey of 850 emergency physicians, 41% said their EHR systems flooded them with Beers Criteria alerts-even for appropriate prescriptions. A 78-year-old on warfarin for atrial fibrillation? The system still warns about bleeding risk. Clinicians get so used to ignoring the alerts that they start overriding them all. One doctor called it “alert fatigue.” And there’s another problem: rigid rules can backfire. A Reddit post from a doctor described how a 68-year-old with strong heart disease risk factors was denied aspirin because the system said “no aspirin after 70.” The patient had no bleeding history. The rule didn’t fit the person.What Works in Practice
The most effective programs share three things:- Multidisciplinary teams-pharmacists, geriatricians, nurses, and social workers working together. Studies show these teams reduce PIMs by 37%, compared to just 22% with computer alerts alone.
- Deprescribing conversations-not just stopping drugs, but talking to patients about why. A 2025 study found that 42% of seniors agreed to stop a medication when the doctor explained the risks in plain language.
- Customized EHR alerts-not blanket warnings. Smart systems now filter alerts by clinical context: “Don’t warn about warfarin if the patient has atrial fibrillation.”

The Bigger Picture: Demographics and Dollars
By 2030, 74 million Americans will be over 65. Right now, 17% of the population is. Medication problems already cost the U.S. healthcare system $528 billion a year. CMS is responding: hospitals that don’t follow geriatric safety protocols face 0.5% reimbursement cuts. The market for tools and software to support this is growing at 14.3% per year. But there’s a gap: only 3.2% of pharmacists specialize in geriatrics. Meanwhile, 16% of all prescriptions go to older adults. We’re training too few experts to care for too many patients.What You Can Do
If you’re caring for an older adult:- Ask: “Are all these medications still needed?”
- Bring a complete list to every appointment-including supplements and OTC drugs.
- Ask if non-drug options exist for pain, sleep, or bladder issues.
- Watch for signs of side effects: confusion, dizziness, falls, nausea, or changes in urination.
- Use the 2023 Beers Criteria and the 2025 Alternatives List together.
- Partner with a clinical pharmacist. Even 0.5 FTE per 20,000 ED visits makes a measurable difference.
- Don’t follow rules blindly. A 70-year-old with no bleeding history and high cardiac risk might still benefit from low-dose aspirin.
What’s Coming Next
By 2026, CMS will expand Measure 238 to track deprescribing-not just prescribing. That means hospitals will be rewarded not just for stopping bad drugs, but for successfully switching to safer ones. The AGS is also developing AI-driven alert systems for EHRs. Instead of bombarding clinicians with every Beers Criteria flag, future systems will use patient history to prioritize the most dangerous interactions. This could cut alert fatigue by half. The future of geriatric care isn’t just about avoiding harm-it’s about rebuilding care around the person, not the pill.What are the most dangerous medications for elderly patients?
The most dangerous medications for older adults include benzodiazepines (like lorazepam), anticholinergics (like diphenhydramine), NSAIDs (like indomethacin), opioids (like meperidine), and certain antipsychotics. These drugs increase risks of falls, confusion, kidney damage, and internal bleeding. The 2023 Beers Criteria specifically flags 139 medications or classes as potentially inappropriate for seniors, with 21 high-risk classes tracked under CMS Measure 238.
What is the Beers Criteria and why does it matter?
The Beers Criteria is a list of medications that should be avoided or used with extreme caution in adults 65 and older. Developed by the American Geriatrics Society and updated every three years, it’s based on clinical evidence and used by hospitals, pharmacies, and insurers. It matters because it helps prevent adverse drug events-leading causes of hospitalization in older adults. As of 2025, it’s integrated into over 87% of Epic EHR systems and is a federal requirement for emergency departments under CMS guidelines.
Can elderly patients stop taking medications safely?
Yes, and often they should. Deprescribing-gradually stopping unnecessary or harmful medications-is a proven strategy to improve safety and quality of life. A 2025 JAMA study found that 42% of seniors agreed to stop a drug when their doctor explained the risks clearly. The AGS Alternatives List (2025) now provides evidence-based non-drug and safer drug options to replace PIMs, making deprescribing more practical and effective.
How do hospitals improve geriatric medication safety?
Hospitals with the best outcomes use multidisciplinary teams-pharmacists, geriatricians, and nurses-who review medications daily. They integrate Beers Criteria alerts into EHRs with smart filters to reduce false alarms. They also use tools like the GEMS-Rx toolkit and deprescribing scripts. Programs that include a clinical pharmacist (0.5 FTE per 20,000 ED visits) cut inappropriate prescribing by over 37%. CMS now requires hospitals to track high-risk drug combinations under Measure 238.
What role do pharmacists play in geriatric medication safety?
Pharmacists are central. They’re the ones who catch dangerous interactions, recommend alternatives, and lead deprescribing efforts. Studies show that programs with pharmacist involvement reduce adverse drug events by 34.7%, compared to just 18.3% with alerts alone. Board-certified geriatric pharmacists (BCGP) are especially valuable-though only 1,247 hold this certification nationwide as of 2025. Their expertise is critical in emergency departments, nursing homes, and primary care settings where older adults are most vulnerable.
Marie Fontaine
February 9, 2026 AT 03:08Ryan Vargas
February 9, 2026 AT 19:46Ashlyn Ellison
February 9, 2026 AT 22:18Scott Conner
February 11, 2026 AT 04:06Alex Ogle
February 12, 2026 AT 21:28Tatiana Barbosa
February 13, 2026 AT 13:55Random Guy
February 14, 2026 AT 12:15Simon Critchley
February 15, 2026 AT 22:00Tom Forwood
February 17, 2026 AT 20:09John McDonald
February 19, 2026 AT 13:06Jacob den Hollander
February 19, 2026 AT 17:19John Watts
February 19, 2026 AT 20:52