More than 1 in 5 people worldwide have a fungal skin infection right now. It’s not rare. It’s not unusual. And it’s not always what you think. You might blame a rash on eczema, sweat, or even an allergic reaction - but it could be a fungus. Two of the most common culprits? Candida and ringworm. Both cause red, itchy skin, but they’re totally different in how they behave, where they live, and how they’re treated.
What’s Actually Growing on Your Skin?
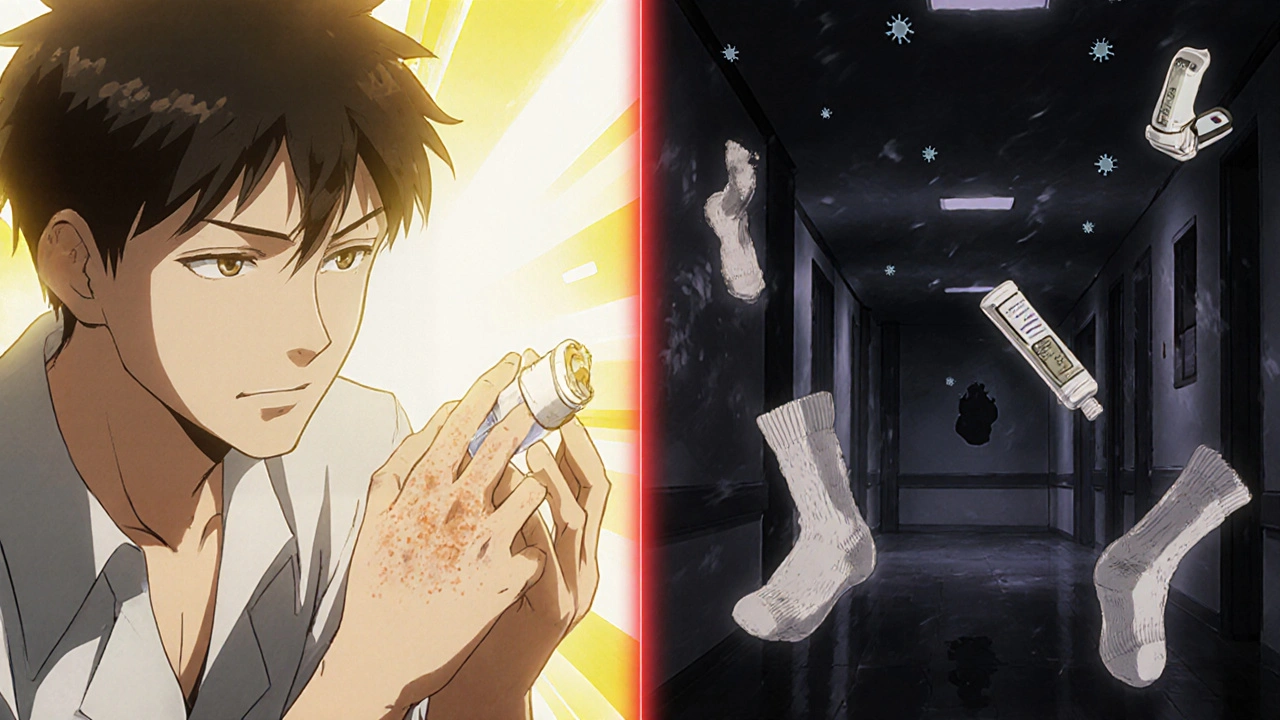
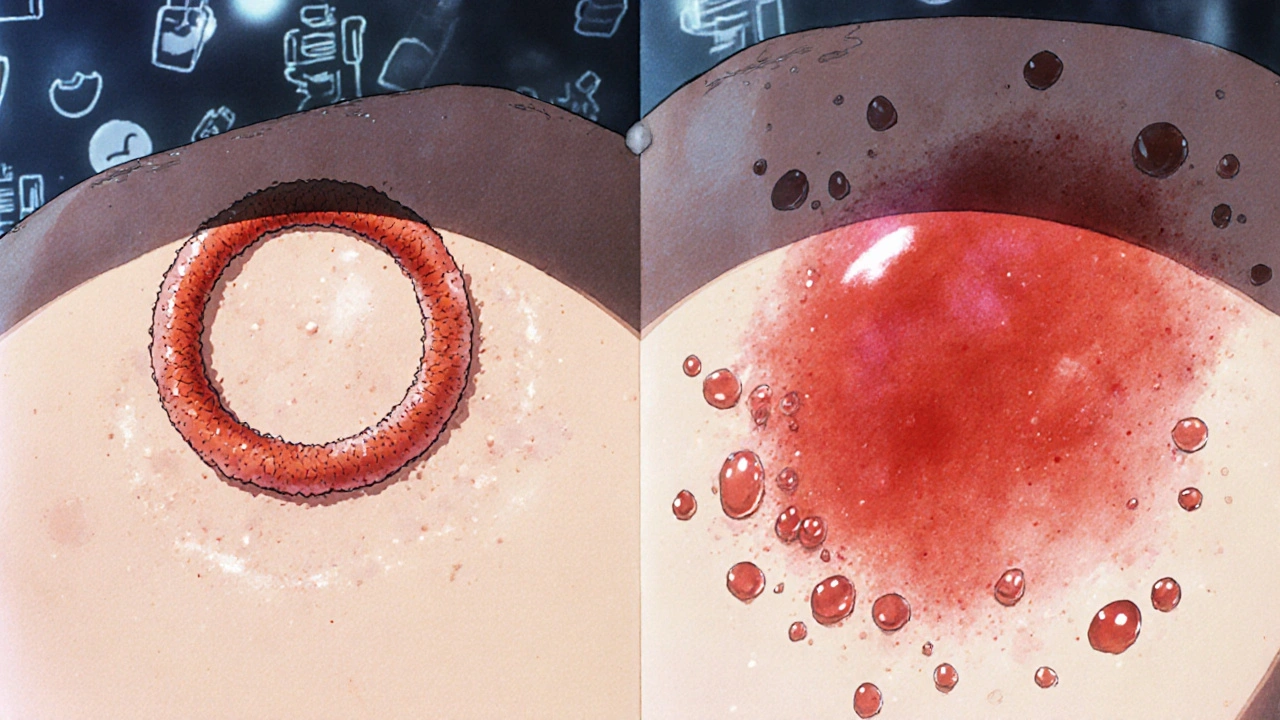
Ringworm isn’t a worm. It’s a fungus. The name comes from the old-school idea that the circular, red, scaly patch looked like a worm curled under the skin. Today, we know it’s caused by dermatophytes - fungi that feed on keratin, the protein in your skin, hair, and nails. The most common type, Trichophyton rubrum, makes up 80-90% of cases. It shows up as a raised, red ring with clearer skin in the middle. You’ll see it on your arms, legs, chest - anywhere the skin is warm and damp.
Candida, on the other hand, is yeast. It’s the same kind that causes thrush or vaginal yeast infections. Normally, it hangs out harmlessly in your gut or on your skin. But when conditions get warm and moist - like under your breasts, in your armpits, or in your diaper area - it multiplies fast. Candida doesn’t form rings. Instead, it creates a bright red, wet, sometimes pimply rash with tiny red dots (satellite pustules) around the edges. It’s common in babies with diaper rash, people with diabetes, or anyone who sweats a lot.
Who Gets These Infections - and Why?
Children under 10 are most likely to get ringworm on the scalp or body. Often, it comes from pets - especially cats and dogs with patchy fur. If your kid pets a stray or even your own cat with a bald spot, they could pick it up. In adults, ringworm on the feet (athlete’s foot) and groin (jock itch) is more common. Locker rooms, shared towels, and tight shoes create the perfect storm.
Candida infections are more tied to your body’s internal state. Diabetes? That raises your risk by 2.5 times. Antibiotics? They kill off good bacteria that normally keep yeast in check. Obesity? Skin folds trap moisture. Immune problems? You’re 3-5 times more likely to get a bad or recurring infection. And yes - wearing synthetic underwear or not drying off after a shower can tip the scales.
How Do You Know It’s Fungal - Not Something Else?
Doctors get it wrong nearly half the time. A 2022 study found primary care providers correctly identified ringworm in only 50-60% of cases. Many patients are told they have eczema or psoriasis - and end up using steroid creams that make the fungus spread. That’s why it’s so important to know what to look for.
Ringworm: circular, scaly, raised border, clears in the center. It often itches but doesn’t ooze. Candida: beefy red, moist, with little red bumps around the edges. It stings more than it itches. Both can be confirmed with a quick test: a scraping of the skin mixed with potassium hydroxide (KOH) under a microscope. The fungus shows up like little threads or spores. Culture tests take weeks, but KOH gives results in minutes.
If you’ve had the same rash for more than two weeks and OTC creams haven’t helped, get it checked. Don’t assume it’s just dry skin.

Topical Antifungals: What Actually Works
For most cases of ringworm on the body or Candida in skin folds, you don’t need pills. Over-the-counter creams work fine - if you use them right.
- Terbinafine (Lamisil): Best for ringworm. Kills fungus, doesn’t just slow it down. Apply twice a day for 1-2 weeks. Cure rate: 70-90%.
- Clotrimazole (Lotrimin): Good for both ringworm and Candida. Apply twice daily for 2-4 weeks. Works well for diaper rash and intertrigo.
- Nystatin: Used mostly for Candida in babies. Comes as cream or powder. Less effective than azoles but safe for long-term use.
Here’s the catch: most people stop using the cream as soon as the redness fades. That’s a mistake. Fungus hides deep in the skin. You need to keep applying for at least a week after the rash looks gone. A 2022 JAMA Dermatology study found only 45% of people finished their full course. That’s why 35% of users report the rash coming back.
When Do You Need Oral Medication?
Topical creams won’t touch nail infections (tinea unguium) or stubborn scalp ringworm. For those, you need pills.
- Terbinafine (oral): First choice for nail fungus. Take 250 mg daily for 6-12 weeks. Works in 80-90% of cases. Side effect? Liver enzymes can rise - your doctor will check them.
- Fluconazole: Used for Candida that won’t quit - especially if it’s in your mouth, throat, or genitals. Takes 1-2 weeks. But resistance is growing. In 2023, fluconazole prescriptions dropped 8% as doctors look for alternatives.
- Ibrexafungerp (Brexafemme): New FDA-approved pill for recurring vaginal yeast infections. Reduces recurrence by half over 48 weeks. Still pricey, but a game-changer for chronic sufferers.
Don’t take oral antifungals without a diagnosis. They’re not harmless. Liver damage, drug interactions, and side effects are real. Use them only when needed.
What About Probiotics and Natural Remedies?
On Reddit and Instagram, thousands of people swear by probiotics for recurring Candida. One June 2023 Instagram poll of 850 users found 65% had fewer flare-ups when they took Lactobacillus supplements alongside antifungals. It makes sense. Good bacteria crowd out yeast. But don’t rely on them alone. Probiotics help - they don’t cure.
Tea tree oil, coconut oil, and apple cider vinegar get lots of buzz. Some small studies show mild antifungal effects, but nothing compares to FDA-approved creams. If you use them, don’t skip your prescribed treatment. And never put undiluted essential oils on broken skin - it can burn.
The Hidden Threat: Drug-Resistant Fungi
There’s a quiet crisis brewing. Fungi are getting smarter. In North America, 5-7% of ringworm strains are now resistant to terbinafine. And then there’s Candida auris - a superbug first spotted in 2009. It’s now in 27 U.S. states. It clings to skin, spreads in hospitals, and resists multiple drugs. It’s not common in healthy people, but it’s deadly for those in ICUs or with weak immune systems.
Doctors are now using newer drugs like olorofim (still in trials) and ibrexafungerp to fight resistant strains. The WHO added five fungal pathogens to its priority list in 2022. That’s a wake-up call. Research funding jumped - $32 million from the NIH in 2023 alone. But for now, the best defense is still early diagnosis and finishing your treatment.
Prevention: Simple Steps That Make a Big Difference
You can’t always avoid fungi - they’re everywhere. But you can make your skin a bad place for them to live.
- Dry off completely after showers - especially between toes, under breasts, and in the groin.
- Wear cotton underwear and loose clothes. Skip synthetic fabrics.
- Don’t share towels, shoes, or combs.
- If your pet has bald patches, get them checked.
- Use antifungal powder in shoes if you’re prone to athlete’s foot.
- Control blood sugar if you have diabetes.
And if you’ve had one fungal infection? You’re more likely to get another. Stay vigilant. A quick check every few weeks can catch a recurrence before it spreads.
Final Thought: Don’t Ignore the Itch
Fungal skin infections aren’t glamorous. They’re messy, frustrating, and often misunderstood. But they’re treatable - if you know what you’re dealing with. Don’t let a rash linger because you think it’s just dry skin. Don’t keep using steroid cream hoping it’ll help. See a doctor. Get tested. Use the right medicine. Finish the course. And remember: you’re not alone. Millions of people deal with this every year. The trick isn’t magic. It’s consistency.
Can ringworm go away on its own?
Sometimes, yes - but it can take months, and you risk spreading it to others or to other parts of your body. Left untreated, ringworm can become chronic or lead to secondary bacterial infections. Antifungal treatment cuts recovery time from months to weeks and reduces the chance of recurrence.
Is Candida contagious?
Candida isn’t typically spread from person to person like a cold. But it can transfer through shared towels, clothing, or surfaces in damp areas like gyms or pools. It’s more about your body’s environment than direct transmission. If someone has a severe Candida infection and you have a weakened immune system, your risk increases.
Can I use the same cream for ringworm and Candida?
Many over-the-counter creams, like clotrimazole, work for both. But terbinafine is more effective for ringworm and less reliable for Candida. If you’re unsure, start with clotrimazole. If it doesn’t improve in 7-10 days, see a doctor. Using the wrong cream can delay healing.
Why does my fungal infection keep coming back?
Recurring infections usually mean one of three things: you didn’t finish your treatment, your environment hasn’t changed (e.g., you still wear sweaty shoes), or you have an underlying condition like diabetes or a weakened immune system. People with diabetes or who take steroids regularly are at higher risk. A doctor can help identify the root cause.
Are antifungal creams safe for babies?
Yes, but only certain ones. Nystatin and mild clotrimazole creams are safe for diaper rash caused by Candida. Avoid strong antifungals like terbinafine on infants unless directed by a pediatrician. Always clean and dry the area thoroughly before applying cream. If the rash doesn’t improve in 3 days, see a doctor.
Do I need to throw away my shoes if I have athlete’s foot?
No, but you should disinfect them. Sprinkle antifungal powder inside, or spray with a solution of 1 part vinegar to 2 parts water. Let them air out in sunlight for a few hours. Replace old, worn-out shoes if they’re always damp. Fungus can survive in shoes for months - so treating the environment is just as important as treating your skin.
Edward Ward
November 15, 2025 AT 05:53It's fascinating how much we misunderstand fungal infections-most people think ringworm is a worm, and Candida is just a ‘yeast issue’ you get from eating too much sugar. But the science is way more nuanced. Dermatophytes are evolved to break down keratin, which is why they target skin, hair, nails-not just damp areas. And Candida? It’s not an invader; it’s a resident that overgrows when the microbiome collapses. Antibiotics, steroids, even stress can trigger it. We treat symptoms, not the imbalance. The real issue isn’t the fungus-it’s the environment we’ve created inside our own bodies and homes.
Jessica Chambers
November 17, 2025 AT 03:54So let me get this straight-we’re supposed to believe that a $10 cream from CVS is the answer to a 27-state superbug crisis? 😏
BABA SABKA
November 18, 2025 AT 09:13Let’s be real-most of these infections are preventable if you stop wearing polyester underwear and stop sharing gym towels like it’s a frat party. I’ve had athlete’s foot since 2018. I stopped using OTC crap and started soaking my feet in saltwater + tea tree oil. No more itching. No more shame. The pharma companies don’t want you to know this works. But here we are.
Ryan Airey
November 19, 2025 AT 01:56Terbinafine cure rates? 70-90%? That’s a marketing lie. I used Lamisil for six weeks. The rash came back worse. My doctor shrugged and prescribed fluconazole. Then I read the FDA warning about liver toxicity. I’m not taking another pill until someone proves this isn’t just a profit-driven cycle of re-infection.
Andrew Eppich
November 20, 2025 AT 06:01It is regrettable that the public discourse surrounding dermatological conditions has devolved into a cacophony of unverified anecdotes and Instagram wellness influencers. The article presents evidence-based clinical guidance. One does not cure a dermatophyte infection with apple cider vinegar, nor does one prevent candidiasis by ‘balancing energy.’ Medical science requires discipline, not dogma.
Jonathan Dobey
November 20, 2025 AT 06:39They’re not just fungi-they’re the vanguard of a silent biological rebellion. The pharmaceutical-industrial complex has spent decades convincing us that skin rashes are ‘minor’-but what if this is the opening salvo? Candida auris doesn’t care about your skincare routine. It doesn’t care about your ‘clean living.’ It’s evolving faster than our regulatory agencies can keep up. We’re living in the age of microbial supremacy. And we’re being fed OTC creams like pacifiers. Wake up. This isn’t about hygiene. It’s about control.
John Foster
November 20, 2025 AT 07:54There’s a deeper truth here that nobody wants to admit: fungal infections are the body’s way of screaming that something is fundamentally off. Not just ‘you didn’t dry off’ or ‘you wore synthetic underwear.’ No. It’s your diet, your sleep, your chronic stress, your gut microbiome in ruins. We treat the surface like it’s a cosmetic issue. But the real infection is systemic. Look at the rise in autoimmune disorders, chronic fatigue, brain fog-all of it correlates with the same modern lifestyle that creates perfect conditions for Candida to thrive. We’re not fighting fungi. We’re fighting ourselves.
Hollis Hollywood
November 21, 2025 AT 14:24I had recurrent jock itch for three years. Tried everything. Then I started using a cotton towel just for my groin, washed it in hot water every day, and stopped wearing tight jeans. Also, I stopped stressing about it. I mean, really-how much energy were you spending worrying about a rash? Once I stopped treating it like a personal failure, it just… faded. I think the shame makes it worse. You’re not broken. You’re just human. And fungi? They’re just doing their job.
Shyamal Spadoni
November 23, 2025 AT 07:18Did you know the CDC is hiding the real stats? The 5-7% resistance rate? That's just the tip. The WHO list? A distraction. Fungi are being weaponized. I work in biotech. I've seen the patents. They're engineering resistant strains to test new drugs. That's why fluconazole is being phased out. They need you to buy the new $400 pill. And don't get me started on the 2023 NIH funding spike-$32 million? That's enough to buy a small country. Who benefits? Always the same people.
Ogonna Igbo
November 23, 2025 AT 22:28Why are we talking about creams and shoes? In Nigeria we have real problems. Fungal infections are common but we don’t have access to Lamisil or even clotrimazole in rural areas. People use ash, lemon, and bitter leaf. Sometimes it works. Sometimes it doesn’t. But no one is talking about how the global health system ignores Africa. You write long articles about KOH tests while our clinics don’t have gloves. This is not science. This is privilege.
ASHISH TURAN
November 25, 2025 AT 20:23One thing people miss: if you’ve had one fungal infection, your skin’s barrier is compromised. It’s not just about hygiene-it’s about rebuilding the skin’s microbiome. I started using a prebiotic moisturizer with oat extract after my last bout. No more recurrence. No fancy drugs. Just supporting the skin’s own defenses. Simple, but it works.
Chris Bryan
November 26, 2025 AT 08:37They say finish your course. But what if the cream is laced with microchips? What if the KOH test is just a cover for DNA harvesting? I don’t trust the system. I don’t trust the labs. I don’t trust the ‘experts.’ I washed my socks in bleach, burned my towels, and moved to a cabin in the woods. No fungus. No doctors. No lies. Maybe the real cure is isolation.