Acetaminophen Overdose Risk Calculator
Critical Warning
The maximum safe daily dose of acetaminophen is 4,000 mg. Exceeding this significantly increases risk of liver failure.
Do not rely solely on this calculator. If you suspect an overdose, seek emergency care immediately.
Total Acetaminophen Daily
Safe Limit
Recommended Actions
- Consult your doctor about safer pain management options
- Track all acetaminophen sources using this calculator
- Never exceed 4,000 mg per day (or 3,000 mg if over 60 years old)
- Always check medication labels for hidden acetaminophen
What Is Fulminant Hepatic Failure?
Fulminant hepatic failure (FHF), also called acute liver failure, doesn’t creep up-it hits like a lightning strike. It happens when a healthy liver suddenly stops working, often within days or even hours. There’s no prior liver disease. No warning. Just jaundice, confusion, and blood that won’t clot. And in nearly half of all cases, it’s caused by something most people think is safe: medications.
Every year in the U.S., about 2,000 people develop this condition. The most common trigger? Acetaminophen. Not the kind you take for a headache once in a while. The kind you take every day for back pain, or mix with painkillers without realizing you’re hitting 6, 8, even 10 grams a day. That’s more than double the safe limit. And when it happens, the liver doesn’t just get tired-it starts dying.
Why Timing Is Everything
Survival isn’t about how sick you are when you get to the hospital. It’s about how fast you get treated. If you get N-acetylcysteine (NAC)-the antidote for acetaminophen overdose-within 8 hours of taking too much, your chances of surviving without a transplant jump to 63%. Wait 24 hours? That number drops to 28%.
Most people don’t realize they’ve overdosed. They think, "I only took what the label said." But many prescription painkillers already contain acetaminophen. Hydrocodone, oxycodone, tramadol-they all come bundled with it. Take two pills for pain, then grab a Tylenol for fever? You’ve just crossed the line. And you won’t feel it until it’s too late.
Red Flags No ER Should Miss
There are three unmistakable signs that your liver has failed:
- Yellow skin or eyes (jaundice)
- Confusion, drowsiness, or personality changes (hepatic encephalopathy)
- Bleeding or bruising easily (coagulopathy)
But here’s what doctors often miss: the early stuff. Persistent nausea with no vomiting. Loss of appetite, even if you’re not sick. A quiet change in behavior-someone who’s usually sharp suddenly can’t focus. Family members notice this first. In 89% of cases, it’s a loved one who says, "Something’s not right."
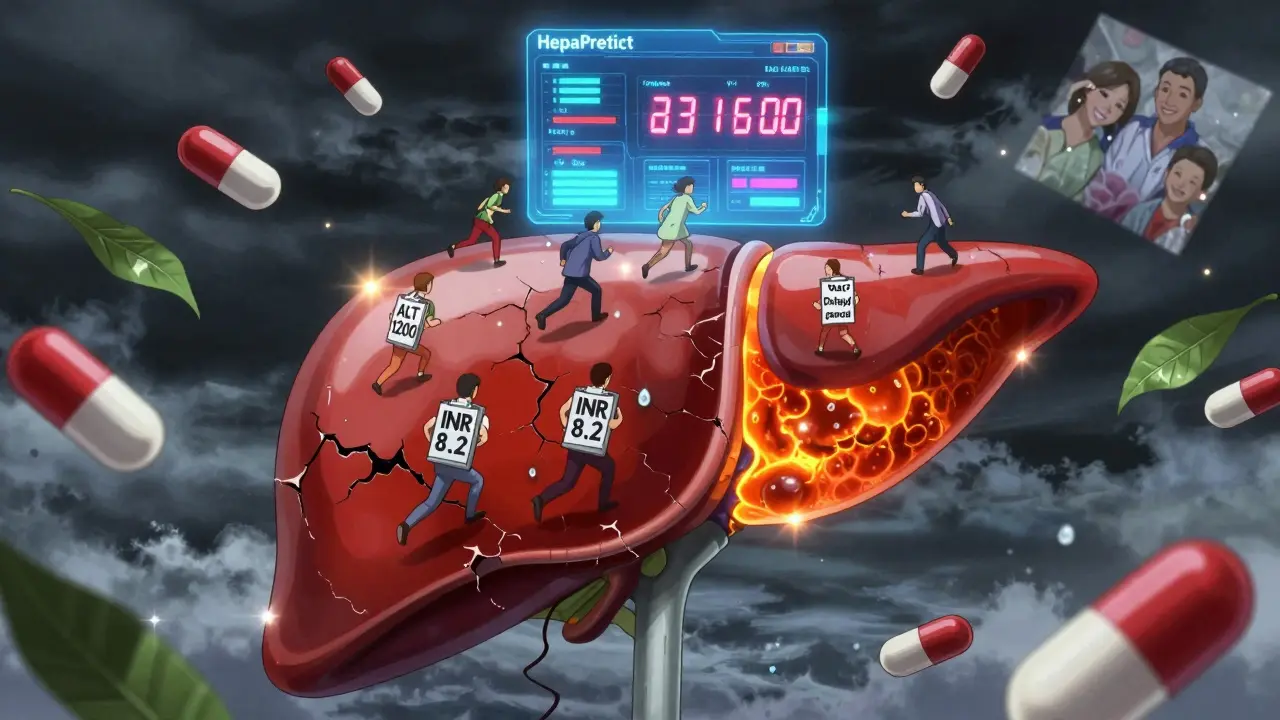
Lab tests confirm it. An ALT level over 1,000 IU/L? That’s a red flare. An INR above 1.5? Your blood is starting to pool instead of clot. And if the INR hits 6.5? Without a transplant, you have a 90% chance of dying. That’s not a guess. It’s from Mayo Clinic’s own data.

Acetaminophen vs. Everything Else
Not all medication-induced liver failure is the same.
Acetaminophen is fast. Most people develop confusion within 72 hours of taking too much. The liver enzymes spike hard. The ALT is way higher than AST. And there’s a tool-called the Rumack-Matthew nomogram-that can predict if you’re in danger based on your blood level and when you took it. It’s accurate. It’s proven. And yet, 23% of people who end up in liver failure with acetaminophen don’t even admit to taking it.
Other drugs? Slower. Messier. Antibiotics like amoxicillin-clavulanate can take weeks. You might think you have the flu. Your ALT might only be 300. But if your bilirubin is over 2 and your ALT is over 3? That’s Hy’s Law. And according to the European Association for the Study of the Liver, that means you need to be in the hospital, with your INR checked every day.
Herbal supplements? They’re the wild card. Green tea extract. Kava. Ashwagandha. People think "natural" means safe. But in the last four years, 42% of supplement-related liver failures in the U.S. came from green tea extract. One woman took 800 mg a day for months. No symptoms. Then-suddenly-she couldn’t stand up. Her INR was 8.2. She needed a transplant.
What Emergency Teams Are Doing Differently
Top hospitals are changing how they screen. At Mayo Clinic, if you walk in with nausea and jaundice, they don’t wait for a history. They check your acetaminophen level immediately. Even if you say you didn’t take it. Even if you’re 70. Even if you’re "just tired."
The Acute Liver Failure Study Group now recommends a 30-minute triage protocol for every ER: test ALT, INR, and acetaminophen level the moment you see jaundice and nausea. No exceptions. That’s how they catch 98.7% of cases.
They also check mental status hourly. Not just "Are you awake?" But: Can you name the president? Can you spell "world" backward? These are the West Haven Criteria. And if your score climbs to grade III or IV? You’re in the transplant zone.
Why So Many Cases Are Missed
Doctors aren’t lazy. But they’re trained to think of common things first. Nausea? Must be stomach flu. Confusion? Could be a UTI. Fatigue? Stress. And when someone says, "I take vitamins," no one thinks to ask which ones. Or how much. Or for how long.
A Johns Hopkins study found 17 cases where people were sent home with a diagnosis of gastroenteritis-when they were actually having drug-induced liver failure. They came back five days later, in full collapse.
And then there’s the "therapeutic misadventure." That’s the medical term for taking the right dose of the wrong combination. A patient on hydrocodone/acetaminophen 5/325 mg four times a day is getting 1,300 mg of acetaminophen per dose. That’s 5,200 mg a day. The limit is 4,000. They didn’t break the rules. They just didn’t know the rules applied to everything they took.
What’s Changing Right Now
Technology is catching up. In 2023, the FDA cleared HepaPredict, an AI system that looks at 17 blood markers and clinical signs to predict liver failure with 89% accuracy-within 24 hours. That’s huge. It doesn’t replace judgment. But it gives doctors a second pair of eyes.
And there’s a new national alert system launching in 2024. Every ER that sees a suspected case must report it within an hour. That way, transplant centers can start preparing before the patient even arrives. In California, this cut time-to-transplant by more than a day.
Even the science is advancing. Researchers found that a tiny molecule called miR-122 rises in the blood just six hours after acetaminophen overdose-long before ALT spikes. In the next few years, ERs might have a rapid blood test that tells them, "Your liver is dying," before you even feel it.
What You Need to Do Now
If you or someone you know is taking any medication-prescription, over-the-counter, or supplement-and starts feeling unusually tired, nauseous, or confused:
- Stop all medications immediately.
- Go to the ER. Don’t wait. Don’t call your doctor first.
- Bring a list of everything you’ve taken in the last 30 days-down to the brand, dose, and how often.
- Ask: "Could this be liver failure? Can you check my acetaminophen level and INR?"
And if you’re on any painkiller with acetaminophen? Add up the total. Is it over 4,000 mg a day? Cut it in half. Talk to your doctor. There are safer options.
Final Thought: It’s Preventable
Fulminant hepatic failure from medications isn’t a mystery. It’s a failure of awareness. We’ve known how to stop it for decades. We know the signs. We have the antidote. We have the tools.
What we’re missing is urgency. People don’t realize that a single extra pill-taken every day-can kill their liver. And doctors don’t always ask the right questions.
But it doesn’t have to be this way. If you know the signs, you can save a life. Your own. Or someone else’s.
What are the first signs of medication-induced liver failure?
The earliest signs are often subtle: persistent nausea, loss of appetite, fatigue, or unexplained confusion. Jaundice (yellow skin or eyes) and easy bruising come later. Family members often notice personality changes-like someone becoming unusually quiet or disoriented-before the patient does.
Can you survive fulminant hepatic failure without a transplant?
Yes, but only if caught early. For acetaminophen overdose, 63% of patients recover without a transplant if treated with N-acetylcysteine within 8 hours. For other drug reactions, survival without transplant drops to 29%. Once INR hits 6.5 or pH falls below 7.3, survival without transplant is less than 10%.
Is acetaminophen the only medication that causes this?
No. While acetaminophen causes nearly half of all cases in the U.S., other common culprits include antibiotics like amoxicillin-clavulanate, antiseizure drugs like valproic acid, and herbal supplements like green tea extract and kava. Even some NSAIDs and statins have been linked. Any medication can cause it-but some are far more likely.
How do doctors know if it’s caused by a drug?
They rule everything else out-viral hepatitis, alcohol, autoimmune disease. Then they look for patterns: timing of symptom onset after starting a new drug, liver enzyme patterns (like ALT > AST in acetaminophen), and whether symptoms improve after stopping the drug. Hy’s Law (ALT/AST >3x ULN with bilirubin >2x ULN) is a major red flag.
Can herbal supplements really cause liver failure?
Absolutely. From 2019 to 2022, 42% of supplement-related liver failure cases in the U.S. involved green tea extract, often taken at doses over 800 mg daily. Kava, comfrey, and weight-loss supplements like those containing pyrrolizidine alkaloids have also caused fatal liver damage. "Natural" doesn’t mean safe.
What should I do if I think I’ve taken too much acetaminophen?
Go to the emergency room immediately-even if you feel fine. Don’t wait for symptoms. Bring the bottle of the medication you took. Tell them exactly how much and when. Ask for an acetaminophen blood level and an INR test. N-acetylcysteine works best if given within 8 hours, but it can still help up to 24 hours after overdose.

Dave Alponvyr
December 16, 2025 AT 19:08Kim Hines
December 18, 2025 AT 11:53Cassandra Collins
December 19, 2025 AT 02:38Joanna Ebizie
December 20, 2025 AT 17:50Kitty Price
December 22, 2025 AT 12:10Arun ana
December 22, 2025 AT 21:56Dan Padgett
December 23, 2025 AT 21:19Ron Williams
December 24, 2025 AT 09:46Hadi Santoso
December 24, 2025 AT 17:29Elizabeth Bauman
December 26, 2025 AT 06:16Josias Ariel Mahlangu
December 26, 2025 AT 14:42Mike Smith
December 27, 2025 AT 03:24Souhardya Paul
December 28, 2025 AT 10:32Dylan Smith
December 28, 2025 AT 19:57