Cardiovascular disease isn’t just one thing. It’s a group of conditions that attack your heart, brain, and blood vessels - often without warning. In the U.S., it kills nearly 800,000 people every year. That’s one in every three deaths. Globally, it’s the number one cause of death. And yet, most of these cases are preventable.
What Exactly Is Cardiovascular Disease?
Cardiovascular disease (CVD) covers a range of problems tied to your heart and blood vessels. The most common type is atherosclerotic cardiovascular disease, or ASCVD. That’s when fatty plaques build up in your arteries, narrowing them over time. This can lead to heart attacks, strokes, or blocked legs (peripheral artery disease). It’s not just about cholesterol. It’s about inflammation, high blood pressure, and how your body handles sugar.Here’s what falls under CVD:
- Coronary artery disease: Clogged arteries feeding your heart. Affects over 18 million U.S. adults.
- Stroke: When blood flow to the brain stops. Around 795,000 Americans have one each year.
- Peripheral artery disease (PAD): Narrowed arteries in your legs. About 6.5 million people over 40 have it.
- Heart failure: Your heart can’t pump well enough. Nearly 6.2 million people live with it.
- Aortic aneurysm: A bulge in your main artery. Can rupture without warning.
These aren’t separate diseases. They’re different symptoms of the same underlying problem: damaged blood vessels.
The Big Risk Factors You Can’t Ignore
You don’t need a genetic lottery ticket to get CVD. The real danger comes from modifiable habits and conditions. The American Heart Association says zip code matters more than genes - meaning where you live, how you eat, and whether you can afford care shapes your risk more than your DNA.Here are the top five risk factors driving CVD today:
- Hypertension: 116 million U.S. adults have high blood pressure. Many don’t even know it.
- Dyslipidemia: Over 71 million people have bad cholesterol levels (LDL-C above 100 mg/dL).
- Diabetes: 11.3% of U.S. adults have it. If you have type 2 diabetes, your risk of heart disease doubles.
- Obesity: Nearly 42% of Americans have a BMI over 30. Fat isn’t just weight - it’s active inflammation.
- Smoking: 11.5% of adults still smoke. One cigarette can damage your endothelium - the inner lining of your arteries - for hours.
And here’s something rarely talked about: depression. People with depression are 30% more likely to develop CVD. And if you’ve had a heart attack, you’re three to four times more likely to become depressed. Mental health and heart health aren’t separate. They’re wired together.
How Doctors Diagnose It Now
Gone are the days of waiting for a heart attack to happen. Today’s guidelines use tools to catch risk before it turns into disaster.The 2023 ACC/AHA guidelines recommend a coronary artery calcium (CAC) scan for people with intermediate risk - that’s a 7.5% to 20% chance of a heart event in 10 years. This non-invasive CT scan shows exactly how much calcium is stuck in your heart arteries. No calcium? Your risk is low. High calcium? You need aggressive action.
And now, AI is stepping in. The new PCE-AI risk calculator improves prediction accuracy by over 12% compared to older models. It looks at more data - not just age and cholesterol, but things like kidney function, inflammation markers, and even social factors.
Screening isn’t just for the elderly. The American Diabetes Association now recommends checking for CVD risk in every person with type 2 diabetes, regardless of age.
What Treatments Actually Work - Today
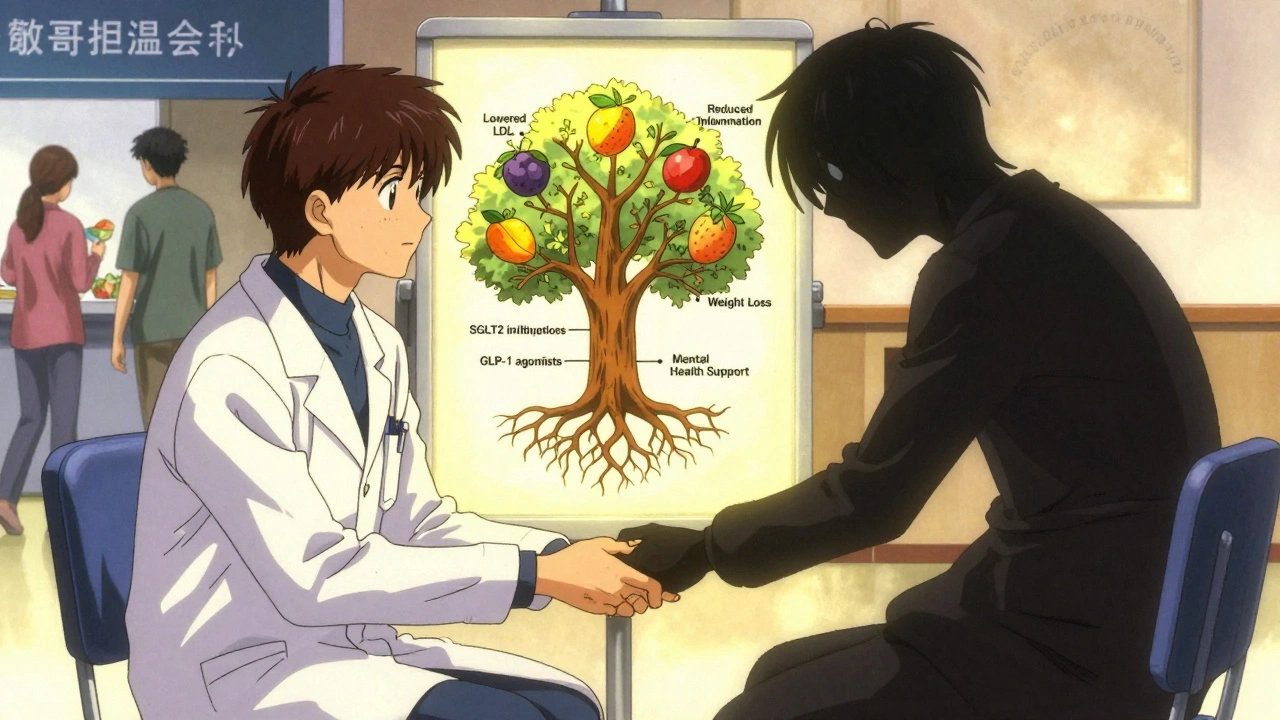
Medication isn’t the only answer. But when used right, it saves lives.Statins still work. They lower LDL cholesterol and reduce heart attacks by up to 30%. But now, we have better options for high-risk patients. The 2025 ADA guidelines say: if you have diabetes and heart disease, aim for an LDL under 55 mg/dL. That’s more aggressive than the ACC/AHA’s 70 mg/dL target.
Two classes of drugs have changed everything:
- SGLT2 inhibitors (like Empagliflozin): Originally for diabetes, they reduce heart failure hospitalizations by 30% and protect kidneys.
- GLP-1 receptor agonists (like Semaglutide): These help you lose weight, lower blood sugar, and reduce heart attacks by 20%.
These aren’t just sugar-lowering pills. They’re heart-protecting tools. And they’re now recommended for people with type 2 diabetes - even if their A1C is normal.
For stroke prevention, dual antiplatelet therapy (aspirin + clopidogrel) is standard after a heart attack or stroke. But only 28% of eligible patients get it. Why? Missed opportunities in clinics, poor follow-up, and cost.
Prevention Isn’t Just About Pills
The most powerful tool against CVD isn’t a prescription. It’s lifestyle.The CDC’s HEARTS package - used successfully in 21 countries - focuses on six pillars:
- Controlling high blood pressure
- Healthy eating (less salt, more plants)
- Smoking cessation
- Access to essential medicines
- Risk-based care (not one-size-fits-all)
- Team-based care (doctors, nurses, pharmacists working together)
Real-world results? CVD deaths dropped 15-25% in places that fully implemented this.
Workplace programs work too. Johnson & Johnson cut CVD risk among employees by 26% over 10 years with wellness programs that included nutrition coaching, fitness incentives, and mental health support.
And if you have prediabetes? Joining the National Diabetes Prevention Program reduces your risk of heart disease by 18%. It’s not magic. It’s structured support - weekly meetings, healthy eating plans, and accountability.
The Hidden Crisis: Inequality and Access
CVD doesn’t hit everyone equally. Black Americans die from heart disease at rates 30% higher than White Americans - even when they have the same cholesterol, blood pressure, and BMI.Why? It’s not biology. It’s access. Black neighborhoods are less likely to have grocery stores with fresh food. More likely to be near highways with pollution. Less likely to have primary care doctors who listen. And more likely to be uninsured or underinsured.
Million Hearts™ - a federal initiative launched in 2012 - is trying to fix this. It pushes the ABCS: Aspirin (when right), Blood pressure control, Cholesterol management, Smoking cessation. Between 2000 and 2019, it helped cut CVD deaths by 21.6%.
But progress is uneven. In 2024, only 54.5% of people with high blood pressure had it under control. That’s not a medical failure. It’s a system failure.
What’s Next? The Future of Heart Health
The 2025 guidelines are pushing a new idea: cardiorenal metabolic syndrome. That’s the recognition that heart disease, kidney disease, and diabetes aren’t separate. They’re one condition with three faces.Doctors are starting to treat them together. A patient with diabetes and early kidney damage? They’re now given an SGLT2 inhibitor - not just for sugar, but for heart and kidney protection.
Mental health is finally being woven into heart care. Pilot programs in Germany show that when depression is screened and treated alongside heart disease, medication adherence improves by 22%.
And the cost? CVD already costs the U.S. $444 billion a year. By 2035, it could hit $1.1 trillion. That’s not just a healthcare crisis. It’s an economic one.
The good news? We know what works. We have the tools. We have the data. What’s missing is consistent action - from clinics, workplaces, and policymakers.
Heart disease isn’t inevitable. Stroke isn’t fate. Vascular damage isn’t just aging. It’s a signal - and we can respond before it’s too late.
What’s the difference between heart disease and cardiovascular disease?
Heart disease refers specifically to problems with the heart - like heart attacks, heart failure, or arrhythmias. Cardiovascular disease is broader. It includes heart disease plus conditions that affect blood vessels - like stroke, peripheral artery disease, and aneurysms. All heart disease is cardiovascular disease, but not all cardiovascular disease is heart disease.
Can you reverse cardiovascular disease?
You can’t erase plaque completely, but you can stabilize it and stop it from growing. Studies show that with aggressive lifestyle changes and medication (like high-dose statins and GLP-1 drugs), plaques can shrink slightly and become less dangerous. The goal isn’t perfection - it’s preventing rupture, which causes heart attacks and strokes.
Is cholesterol the main cause of heart disease?
Cholesterol - especially LDL - is a major player, but not the only one. Inflammation, high blood pressure, insulin resistance, and smoking all damage the artery lining. Cholesterol then gets trapped in those damaged areas. Think of it like rust on a pipe: the rust (cholesterol) builds up because the pipe (artery) is already damaged. Fixing the damage matters as much as lowering cholesterol.
Do I need a CAC scan if I feel fine?
If you’re between 40 and 75 and have risk factors - like high blood pressure, diabetes, smoking, or a family history - yes, it’s worth considering. Many people with silent plaque feel perfectly fine until they have a heart attack. A CAC scan gives you real data, not guesswork. If your score is zero, your risk is very low. If it’s high, you can take action before it’s too late.
Are newer drugs like Ozempic really good for the heart?
Yes. Semaglutide (Ozempic, Wegovy) and similar GLP-1 drugs reduce heart attacks, strokes, and heart failure hospitalizations by 20% in high-risk patients - even if they don’t have diabetes. They work by lowering blood sugar, reducing weight, decreasing inflammation, and improving blood pressure. They’re no longer just weight-loss drugs. They’re heart-protecting tools.
How does depression affect heart health?
Depression raises stress hormones like cortisol, which increases blood pressure and inflammation. It also leads to poor sleep, less exercise, and worse diet choices. People with depression are less likely to take their meds or show up for checkups. Studies show treating depression alongside heart disease improves survival rates and medication adherence by up to 22%.
What’s the best diet to prevent cardiovascular disease?
There’s no single ‘best’ diet, but the most effective ones share common traits: lots of vegetables, fruits, whole grains, beans, nuts, and fish. Low in added sugar, refined carbs, and processed meats. The DASH diet and Mediterranean diet are the two most proven. One study showed people following a Mediterranean diet had 30% fewer heart events over five years compared to a low-fat diet.
Can I prevent CVD if it runs in my family?
Yes. Genetics might load the gun, but lifestyle pulls the trigger. Even if both your parents had heart attacks before 50, you can still cut your risk by 50% or more by not smoking, staying active, eating well, and managing blood pressure and cholesterol. Family history means you need to be more vigilant - not helpless.
What You Can Do Today
You don’t need to wait for a doctor’s appointment to start protecting your heart.- Get your blood pressure checked - even if you feel fine.
- Ask your doctor about your LDL cholesterol and whether a CAC scan makes sense for you.
- If you have diabetes, ask about SGLT2 inhibitors or GLP-1 agonists - even if your A1C is fine.
- Move for 30 minutes most days. Walk, dance, garden - just move.
- Swap one processed snack for a handful of nuts or fruit.
- Check in on your mental health. If you’re feeling down, talk to someone.
CVD doesn’t strike suddenly. It creeps in. But so can change. Start small. Stay consistent. Your heart doesn’t need perfection - it needs you to show up.

Bruno Janssen
December 14, 2025 AT 08:01Emma Sbarge
December 16, 2025 AT 00:40Tommy Watson
December 16, 2025 AT 19:57Michael Gardner
December 17, 2025 AT 02:31Willie Onst
December 19, 2025 AT 01:29Jennifer Taylor
December 20, 2025 AT 01:42Shelby Ume
December 20, 2025 AT 17:41Jade Hovet
December 22, 2025 AT 15:43nithin Kuntumadugu
December 24, 2025 AT 13:28Harriet Wollaston
December 25, 2025 AT 07:18Lauren Scrima
December 26, 2025 AT 23:44sharon soila
December 27, 2025 AT 11:12nina nakamura
December 29, 2025 AT 06:52Constantine Vigderman
December 30, 2025 AT 09:57