When you're on treatment for osteoporosis, waiting a year or two to see if your bone density improves can feel like flying blind. You take your pills, you do your exercises, but how do you know it’s actually working? That’s where bone turnover markers come in. These aren’t fancy sci-fi tools-they’re simple blood tests that tell you, in weeks, whether your treatment is doing its job. And unlike DXA scans that measure bone density over time, bone turnover markers show you what’s happening right now inside your bones.
What Are Bone Turnover Markers?
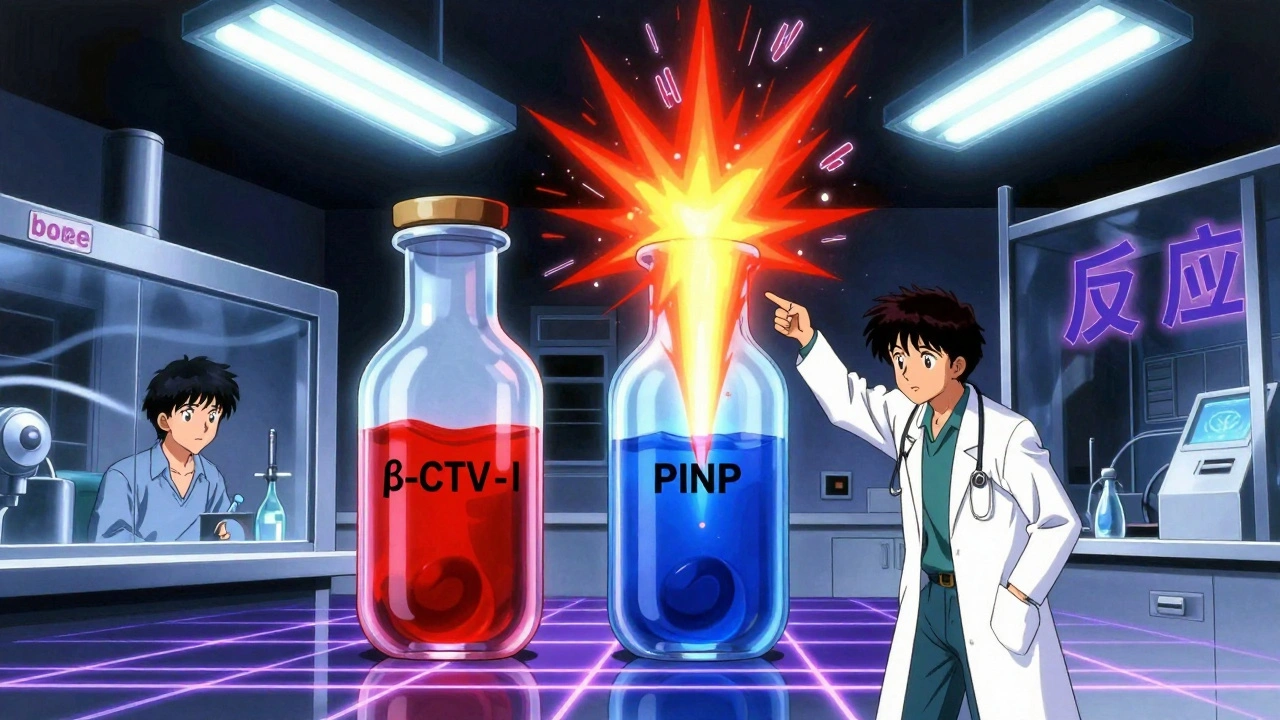
Your bones aren’t static. They’re constantly being broken down and rebuilt-a process called remodeling. When bone is broken down (resorption), fragments of collagen and other proteins spill into your bloodstream. When new bone is made (formation), the body produces specific proteins as building blocks. These fragments and proteins are called bone turnover markers (BTMs). There are two main types:- Resorption markers: Show how fast bone is being broken down. The gold standard is β-CTX-I (beta-C-terminal telopeptide of type I collagen).
- Formation markers: Show how fast new bone is being made. The most reliable is PINP (procollagen type I N-terminal propeptide).
Why Use Them Instead of Just a DXA Scan?
DXA scans are the gold standard for diagnosing osteoporosis. But they’re slow. It takes 12 to 24 months to see a meaningful change in bone density-even if your treatment is working perfectly. That’s a long time to wonder if you’re wasting your time. Bone turnover markers change much faster. Within 3 to 6 weeks of starting treatment, you’ll see shifts in PINP and β-CTX-I levels. By 3 months, the changes are clear enough to judge response. For example:- If you’re on a bisphosphonate (like alendronate or zoledronic acid), your β-CTX-I should drop by more than 30% in 3 months.
- If you’re on teriparatide (an anabolic drug), your PINP should rise by 70-100% in the same window.
How Are They Measured? The Rules Matter
These tests aren’t like a regular cholesterol check. Getting accurate results requires strict rules. For β-CTX-I:- You must fast overnight (no food or drink except water).
- Sample must be taken between 8 and 10 a.m.-CTX levels swing up to 40% during the day.
- Don’t eat for at least 2 hours before the test-eating can spike CTX by 20-30%.
What Counts as a Good Response?
Not every change means something. There’s a threshold called the least significant change (LSC)-the smallest drop or rise that’s real, not just lab noise.- For β-CTX-I: A change of 25% or more is considered meaningful.
- For PINP: A change of 20% or more is meaningful.
- On antiresorptive drugs (bisphosphonates, denosumab): A >30% drop in β-CTX-I or >35% drop in PINP at 3 months = good response.
- On anabolic drugs (teriparatide, romosozumab): A 70-100% rise in PINP at 3 months = good response.
- You’re not taking your medication regularly.
- Your body isn’t absorbing it properly (common with oral bisphosphonates if you eat too soon after taking them).
- You have another condition affecting bone metabolism-like kidney disease or hyperparathyroidism.
Who Should Get Tested?
Not everyone needs BTMs. But they’re especially useful in these cases:- You’re starting a new osteoporosis drug and want to know if it’s working before your next DXA scan.
- You’ve had a fracture despite being on treatment-time to check if you’re responding.
- You’re having side effects and your doctor wants to see if the drug is even active in your system.
- You’re on long-term bisphosphonates and your doctor is considering a drug holiday. BTMs can help decide when it’s safe to pause.
- You have chronic kidney disease (CKD). Standard markers like PINP and β-CTX-I can be misleading in CKD. Alternatives like bone alkaline phosphatase (BALP) or TRACP5b are better here.

Limitations and Pitfalls
BTMs aren’t perfect. Here’s what you need to know:- They reflect overall bone activity, not density at a specific site. A high resorption marker doesn’t tell you if your hip or spine is weakening.
- Biological variability is high. Your levels can jump 20-60% based on time of day, food, exercise, or even menstrual cycle in premenopausal women.
- Reference ranges are mostly based on Caucasian populations. Asian individuals often have 15-20% lower baseline CTX levels. African populations show 10-15% higher PINP. Labs are still catching up to these differences.
- They’re not used for diagnosis. You still need a DXA scan to confirm osteoporosis.
What’s Next for Bone Turnover Markers?
The field is evolving fast. In 2024, the American Association of Clinical Endocrinologists is expected to update its guidelines to include BTMs as a routine part of osteoporosis management. Researchers are also looking at:- Using BTMs to personalize treatment duration-stopping drugs earlier in responders, switching faster in non-responders.
- Point-of-care tests in development that could give results in minutes, not days.
- Better reference ranges for non-Caucasian populations.
- Linking BTM trends to actual fracture risk over time, not just short-term changes.
Putting It All Together: Your Action Plan
If you’re on osteoporosis treatment, here’s what you should ask your doctor:- Can we test my PINP and β-CTX-I before I start treatment?
- Can we repeat the test exactly 3 months after I begin?
- What are my target changes? (More than 30% drop for resorption drugs, 70%+ rise for anabolic drugs.)
- Will we use the same lab for all tests?
- Do I need to fast? What time should I come in?
Are bone turnover markers better than DXA scans for monitoring osteoporosis treatment?
No, they’re not better-they’re different. DXA scans measure bone density and are the gold standard for diagnosing osteoporosis and tracking long-term changes over 1-2 years. Bone turnover markers show how active your bones are right now. They detect treatment response in 3-6 weeks, while DXA takes much longer. Use them together: BTMs for early feedback, DXA for final confirmation.
Can I get bone turnover markers tested at any lab?
Not all labs are equal. These tests require specific methods and strict protocols. Only about 65% of U.S. labs follow international standards. Ask your doctor which lab they use and whether it follows IFCC guidelines. Always use the same lab for all your tests to ensure accurate comparisons over time.
Do I need to fast before a bone turnover marker test?
Yes, for β-CTX-I. You must fast overnight and avoid food for at least 2 hours before the test. Eating can raise CTX levels by 20-30%, making results unreliable. PINP is less affected, but for consistency, it’s best to fast and test in the morning (8-10 a.m.) for both markers.
What if my bone turnover markers don’t change after 3 months?
It could mean you’re not taking your medication properly, your body isn’t absorbing it, or you have another condition like kidney disease. Your doctor may check your adherence, review your dosing schedule, or test for other issues. In some cases, switching to a different drug-like from an oral bisphosphonate to an injection-might be needed.
Are bone turnover markers covered by insurance?
Yes, in the U.S., Medicare covers PINP (CPT 83970) and β-CTX-I (CPT 83935) for osteoporosis monitoring. Private insurers are increasingly following suit. Costs are low-around $30 per test. If your insurer denies coverage, ask your doctor to appeal using the 2023 IOF/ESCEO guidelines as evidence of medical necessity.

Maria Elisha
December 10, 2025 AT 01:59Ugh, another wall of text. Can we just get a summary? I came here for info, not a textbook.
Angela R. Cartes
December 10, 2025 AT 22:52LOL at people thinking these markers are magic. 😒 I’ve seen so many patients get stressed over numbers that don’t even mean anything. DXA is the only thing that matters. 🤷♀️
Lisa Whitesel
December 11, 2025 AT 16:23Don't waste your money on these tests. Labs are inconsistent and most doctors don't know how to interpret them. You're just paying for anxiety. End of story.
Arun Kumar Raut
December 12, 2025 AT 20:40This is actually super helpful. I'm from India and we don't talk much about bone health here. My mom has osteoporosis and we never knew what to look for after she started her meds. Now I know to ask for PINP and CTX tests. Thanks for breaking it down simply.
Larry Lieberman
December 14, 2025 AT 18:35Wait so if I'm on teriparatide and my PINP jumps 80% in 3 months, does that mean I'm basically building bone like a superhero? 🦸♂️💥
Sabrina Thurn
December 15, 2025 AT 14:02For clinicians: BTMs are underutilized but high-value tools. The 2023 IOF/ESCEO guidelines clearly endorse PINP and β-CTX-I as reference markers. The LSC thresholds are well validated. The real barrier is lab standardization and clinician education-not the science. If you're not using them, you're managing osteoporosis in the dark.
Tiffany Sowby
December 15, 2025 AT 14:30Of course Americans think they have all the answers. In Europe we've been doing this for years. Here you guys still think a pill is enough. 🙄
Ronald Ezamaru
December 15, 2025 AT 21:57As someone who's lived in both the US and Japan, I can say the cultural differences in bone health awareness are huge. In Japan, they screen women routinely after 50 and track markers closely. Here, it feels like we wait until someone breaks a hip before anyone cares. This post is a step in the right direction.
Ryan Brady
December 16, 2025 AT 16:12Why are we letting labs run the show? If the government spent half as much on bone health as they do on space rockets, we wouldn't need to guess. Also, why do these tests cost $30? That's a coffee. This is healthcare fraud.
Iris Carmen
December 18, 2025 AT 07:43i just got my btm results and my ctx dropped 40% so im probs not gonna break a bone anytime soon 😌
Stacy Tolbert
December 18, 2025 AT 08:01My doctor said these tests are pointless and that I should just wait for my next DXA. But I did them anyway because I read this. My PINP went up 92%. I feel like I just won the bone lottery. Thank you for making me feel less crazy.